Posted on February 27, 2012 by Archer USMLE Reviews
326) A 55 year old african-american man presents to your office with complaints of shortness of breath that has slowly progressed over the past several months. He also reports chest pain which in non-pleuritic in nature. He has lost about 10lbs weight in the past three months. He has changed several jobs but he currently works as a sales representative for a drug company. On examination, his temperature is 100F, Pulse 98/min, RR 20/min and Blood Pressure 100/60 mm HG. He is in mild distress due to shortness of breath. On chest examination, there is dullness to percussion over the right side of the chest. No masses are palpable. Laboratory investigations reveal WBC 8k/μl with normal differential, Hgb 10.5gm%, Platelets 550k/μl, Calcium 11.2gm% ( (Normal 8.9 to 10.5 mg%)
A chest-x-ray is shown below:

Which of the following element in the history would be most helpful in making a presumptive diagnosis of his presentation?
A) Smoking
B) Family history of Cancer
C) Bone pain
D) Flank pain and Hematuria
E) Previous Occupation
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer pulmonology, archer step 3 pulmonology, USMLE STEP 3 PULMONOLOGY | 11 Comments »
Posted on February 26, 2012 by Archer USMLE Reviews
325 ) A 87 year old Caucasian man is evaluated in your office for progressive hearing loss. He reports defective hearing on both sides that started more than a year ago and has gradually worsened. The problem is particularly worse when he is in a crowded or noisy environment. He also reports frequent occurrence of roaring sounds and sounds similar to “ringing bells” in his ears. On otoscopic examination, he has mild cerumen impaction in bilateral ears. The Tympanic membranes are intact. Which of the following is the most characteristic feature seen with this condition?
A) Inability to hear “Vowel” sounds in the speech
B) Audiogram showing bilateral high-frequency sensory-neural hearing loss
C) Weber Test showing lateralization towards Right ear
D) A negative Rinne test
E) Otosclerosis
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer ENT, aRCHER GERIATRICS, audiometry evaluation, deafness, ear nose throat dosorders, ENT MCQs, geritrics mcqs, hearing loss, usmle ent mcq, USMLE STEP 3 ENT, usmle step 3 geriatrics, weber and rinne tests | 12 Comments »
Posted on February 26, 2012 by Archer USMLE Reviews
324) A 45 year old woman with history of Rheumatoid Arthritis presents to the emergency room increasing pain and swelling in her joints. She reports progressively increasing pain and stiffness of her bilateral wrist joints over the past two weeks. She now developed rapidly increasing pain and swelling in her right knee which prompted this Emergency Room visit. Her medications include Ibuprofen and Methotrexate. On examination, she is afebrile. There is mild swelling and tenderness in bilateral wrist joints. Right knee is warm, swollen and tender. Flexion and extension of the right knee are severely painful. Laboratory investigations are as follows:
WBC 9.0k/µl
Differential: Neutrophils 65%, Lymphocytes 24%, Monocytes 7%
Hemoglobin 11.5 g/dL ( Normal = 13.0 to 16.5 gm%),
Mean cell volume (MCV) 84 fL
Platelet count 510k/µl ( Normal 180 to 350k⁄μl )
ESR : 70 mm/hr
Which of the following is the most appropriate next step in management?
A) Pulse Methyl Prednisolone
B) Oral Prednsione
C) Arthrocentesis
D) Discontinue Methotrexate and start Infliximab
E) Intra-articular Glucocorticoids
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer Rheumatology, Rheumatoid arthritis, USMLE step 3 Rheumatology | 9 Comments »
Posted on February 26, 2012 by Archer USMLE Reviews
323) A 65 year old man is evaluated in your office for slowly progressing involuntary shaking movements in his hands. He noticed these movements about 10 months ago which have slightly worsened now. Occasionally, he was told by his wife that his head shakes as well. The movements have led him to feel socially embarrassed because they are worse when he attempts to write or hold a cup of coffee or fasten a shirt button. He denies any tremors in his legs. He denies any problems with his gait or muscle pain or stiffness. He reports drinking wine on daily basis since the tremors have started because he thinks alcohol appears to improve the tremors. He denies using any medications. There is no family history of tremors or seizures. On examination, he appears comfortable. Tremors are visible bilaterally with his arms outstretched and they are increased when asked to hold a cup filled with water. His handwriting is large and tremulous. Gait is normal with normal arm-swing. There are no other neurological deficits. Routine chemistry panels including TSH and Liver function tests are normal. Which of the following is the most appropriate next step in management?
A) MRI brain with contrast
B) Vitamin B12 level
C) Trial of Dopamine Agonist
D) Initiate Propranolol Therapy
E) Serum Cerulopalsmin level
F) Start oral Primidone
Filed under: Uncategorized, USMLE Test Prep | Tagged: archer neurology, neurology mcqs, neurology usmle mcqs, parkinson tremor, usmle step 3 neurology | 13 Comments »
Posted on February 26, 2012 by Archer USMLE Reviews
322) A 45 year man is evaluated in emergency department for severe cough accompanied by bloody expectoration. Cough is of 4 month duration associated with sputum production but he is worried because of the new change in the character of his sputum which is now frankly bloody. He reports a weight-loss of 10 lbs in the past two months. He has intermittent nigh-sweats and low grade fever on a daily basis. On examination, his temperature is 100F, Pulse 98/min, RR 20/min and Blood Pressure 100/60 mm HG. He appears cachectic and in moderate distress due to cough. On auscultation, high-pitched bronchial breath sounds are heard in the right upper chest.
A chest-x-ray is shown below:

The patient is admitted and is placed on respiratory, negative-pressure isolation. HIV rapid test is positive. Sputum smears for Acid Fast Bacilli (AFB) are positive. A CD4 count is 155/μl ( Normal = 650 to 1150/µl). Which of the following is the most appropriate next step in management at this time?
A) Bronchoscopy and send bronchial washing for clutures
B) Start Multi-Drug anti-tuberculosis Therapy alone
C) Start Highly Active Antiretroviral Therapy (HAART) plus Multi-drug Anti-TB therapy
D) Start HAART and await sputum for AFB identification and sensitivity testing
E) Start Clarithromycin for Mycobacterium Avium Intracellulare (MAC)
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer Infectious Diseases, Archer pulmonology, USMLE STEP 3 INFECTIOUS DISEASES, USMLE STEP 3 PULMONOLOGY | 39 Comments »
Posted on February 7, 2012 by Archer USMLE Reviews
321) A 45 – year-old obese woman presents to your office complaining of a skin lesion on her left shin. This lesion started spontaneously 3 weeks ago and appeared like a small bruise. Over the past two weeks, the lesion has enlarged and the overlying skin has become hardened and raised with reddish border. There is no pain or itching. She denies any recent trauma. She lives in Texas but one month ago, she traveled to New England region to visit a friend. She is sexually active with one partner and occasionally, uses condoms.. Her past medical history is unremarkable. On physical examination, there is an oval shaped lesion on her left shin. The border is indurated and red in color with yellowish, atrophic appearance in the center. An image of the lesion is shown below:

Which of the following investigations should be ordered next?
A) Lyme serology
B) Hemoglobin A1C
C) Anti-Myeloperoxidase ( P-ANCA)
D) Colonoscopy
E) Herpes Simplex Virus (HSV) Serology
Filed under: Uncategorized, USMLE Test Prep | Tagged: archer dermatology, dermatology usmle, dermatology usmle step 3 questions, USMLE STEP 3 DERMATOLOGY, usmle step 3 dermatology images | 22 Comments »
Posted on February 7, 2012 by Archer USMLE Reviews
320) A 65 – year-old woman is evaluated in your office during a follow-up visit. Her medical problems include Diabetes mellitus type II and hypertension. She is being managed on oral metformin, glyburide and hydrochlorthiazide. Her most recent hemoglobin A1C is 6.5%. Her urine was negative for microalbumin three months ago. Her past medical history is significant for hospitalization for angioedema which occured after initiation of Enalapril three years ago. Physical examination is unremarkable. The patient requests if she can be started on Angiotensin Receptor Blocker ( ARB) because she read about its beneficial effects in preventing kidney damage in diabetics. Which of the following is the most appropriate response?
A) “You are correct. I will start you on ARB”
B) ” You can not be started on ARB because of history of Angioedema”
C) “You can start ARB but need pre-medication with steroids”
D) ” You can start ARB but there is a small risk of Angioedema”
E) ” Hydralazine/ Nitrate combination offers similar reno-protective effect as ARB”
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, ARCHER NEPHROLOGY, dr.red nephrology lecture, USMLE STEP 3 CARDIOLOGY, usmle step 3 nephrology | 9 Comments »
Posted on February 7, 2012 by Archer USMLE Reviews
319) A 64-year-old man with history of diabetes mellitus and end-stage renal disease is admitted for complaints of weakness and contractures in his extremities associated with tight and thickened skin. He denies any past history of finger or toe discoloration on exposure to cold. He is dialysis dependent and undergoes hemodialysis three times in a week. His most recent dialysis was a day ago. His symptoms started 3 days prior to presentation and have progressively worsened. Three weeks prior to admission , the patient had a transient ischemic attack. An MRI with Gadolinium performed at that time did not reveal any abnormalities. He denies any neurological symptoms at this time. The patient’s medications upon admission include Aspirin, Insulin Glargine and Lisinopril. On physical examination, the patient appears chronically ill. He is afebrile, blood pressure 120/70 mmHg and pulse rate was 82/minute. Skin examination reveals diffuse nonerythematous thickening and tightening of the skin over the abdomen, arms and legs. Chest and the face are spared. There are contractures in upper and lower extremities extremely limiting the range of motion of the involved joints. Erythrocyte sedimentation rate and C-reactive protein are elevated. Calcium is 8.0mg% and phosphorous 4mg% with calcium – phosphorous product of 32. An image of his upper extremity is shown below

Which of the following is the most likely diagnosis?
A) Systemic sclerosis
B) Calciphylaxis
C) Nephrogenic Systemic Fibrosis
D) Cryoglobulinemia
E) Eosinophilc Fascitis
Filed under: Uncategorized, USMLE Test Prep | Tagged: archer dermatology, ARCHER NEPHROLOGY, dermatology usmle, dermatology usmle step 3 questions, dr.red nephrology lecture, USMLE STEP 3 DERMATOLOGY, usmle step 3 dermatology images, usmle step 3 nephrology | 10 Comments »
Posted on January 30, 2012 by Archer USMLE Reviews
318) A 55 year old woman underwent a debulking surgery with total abdominal hysterectomy, Salpingo-oophorectomy, omentectomy and appendicectomy for a recently diagnosed Stage IIIC Epithelial Ovarian Cancer. Her intra-operative course was complicated by severe blood loss and she received about 15 units of Packed Red Blood Cells. She is currently in the intensive care unit. Six hours after surgery, her blood pressure drops to 80/50 mm Hg. On examination, she is afebrile. She is drowsy but can be awakened. She denies any chest pain or shortness of breath. She has muscle tremors. Chest is clear to auscultation. Abdominal sutures are intact with no clinical evidence of Hematoma. An electrocardiogram is shown below:

Which of the following is the most likely explanation of the patient’s acute findings?
A) Hyperkalemia
B) Acute Myocardial Infarction
C) Circulatory Overload
D) Transfusion Associated Acute Lung injury
E) Citrate Toxicity
Filed under: Uncategorized, USMLE Test Prep | Tagged: ARCHER ACID-BASE, Archer cardiology, ARCHER FLUID AND ELECTROLYTES, Archer hematology, ARCHER NEPHROLOGY, dr.red nephrology lecture, Hematology, USMLE STEP 3 CARDIOLOGY, USMLE step 3 Hematology, usmle step 3 nephrology | 5 Comments »
Posted on January 30, 2012 by Archer USMLE Reviews
317) A 68-year-old african-american man with history of NYHA Class III congestive heart failure presents to your office for a follow up visit. His other medical problems include Hypertension, Stage II chronic kidney disease and Coronary artery disease. During his office visit three months ago , she was noted to have moderate hyperkalemia. At that time, his medications were adjusted which involved discontinuation of spironolactone and dose-reduction of ACE inhibitor. His other medications included Atenolol and Aspirin. She reports that she was admitted to hospital two weeks ago with severe hyperkalemia. He denies any complaints at this time. A serum potassium level is 4.5mEq/l , serum creatinine 1.8mg% and most recent echocardiogram revealed a left ventricular ejection fraction of 35% . His current medications include Atenolol, Hydrochlorthiazide and Aspirin. Which of the following is the most appropriate next step?
A) Re-start ACE inhibitor at a lower dose
B) Start Angiotensin Receptor Blocker (ARB)
C) Start Hydralazine and Isosorbide
D) Continue current medications
E) Start Spironolactone
Filed under: Uncategorized, USMLE Test Prep | Tagged: ARCHER ACID-BASE, Archer cardiology, ARCHER FLUID AND ELECTROLYTES, ARCHER NEPHROLOGY, dr.red nephrology lecture, USMLE STEP 3 CARDIOLOGY, usmle step 3 nephrology | 8 Comments »
Posted on January 30, 2012 by Archer USMLE Reviews
316) A 72-year-old man was admitted to the hospital with right leg deep vein thrombosis. He has a history of prostate cancer, well-controlled diabetes and mild renal insufficiency. His baseline creatinine is usually between 1.4 to 1.6mg%. His laboratory investigations at admission were normal except for increased creatinine at 1.4mg% . Venous doppler showed leg femoral deep vein thrombosis in femoral vein. He was started on Heparin drip and oral warfarin. Three days after admission, the patient develops persistent hyperkalemia (6.5 to 7.0 mEq/l). Rest of his electrolytes are normal and renal function is at his baseline. His INR ( International Normalized Ratio) is 1.4. There are no EKG abnormalities. His Urine Osmolality is 300mOsm/kg, Urine K 20 mmol/L and Serum Osmolality 280 mOsm/kg. He is given insulin and dextrose therapy however, hyperkalemia persists. Which of the following is the most appropriate next step in management?
A) Start Kayexalate
B) Discontinue Heparin and Start Enoxaparin
C) Discontinue Heparin and place Green field filter
D) Hemodilaysis
E) Intravenous Sodium bicarbonate
Filed under: Uncategorized, USMLE Test Prep | Tagged: ARCHER ACID-BASE, Archer emergency medicine, ARCHER FLUID AND ELECTROLYTES, ARCHER NEPHROLOGY, dr.red nephrology lecture, usmle step 3 nephrology | 8 Comments »
Posted on January 30, 2012 by Archer USMLE Reviews
315) A 64-year-old man with history of diabetes mellitus is evaluated in your office during a follow-up visit . He was admitted to the hospital one week ago because of incidentally discovered high serum potassium of 7.0mEq/L on his routine labs. He has history of hypertension and Stage I chronic kidney disease . His medications prior to the hospital admission included glyburide and enalapril. However, Enalapril was discontinued and he was started on hydrochlorthiazide during that admission. He denies any complaints at this time. A serum potassium level is 4.5mEq/l , serum creatinine 1.8mg% and urinalysis reveals proteinuria. 24 hour urine collection reveals 300mg proteinuria/24hrs. Which of the following is the most appropriate next step?
A) Re-start Enalapril at 50% of previous dose
B) Start Losartan
C) Start Hydralazine and Isosorbide
D) Start Spironolactone
E) Renal biopsy
Filed under: Uncategorized, USMLE Test Prep | Tagged: ARCHER ACID-BASE, ARCHER FLUID AND ELECTROLYTES, ARCHER NEPHROLOGY, dr.red nephrology lecture, usmle step 3 nephrology | 10 Comments »
Posted on January 30, 2012 by Archer USMLE Reviews
314) A 70-year-old man presented to the Emergency room with a 2-day history of increased thirst and frequency of urination. He reports generalized muscle weakness. His past medical history is significant for hypertension, diabetes mellitus and Stage III chronic kidney disease. His medications include Insulin Glargine, Lispro insulin, Enalapril , Atenolol and Spironolactone. Laboratory investigations reveal
Blood glucose 400mg%
Sodium 130 mEq/L
Potassium 7.5 mEq/L
Bicarbonate 26mEq/L
Chloride 100mEq/L
Creatinine 4.2mg%
An electrocardiogram is shown below:

Which of the following is the most appropriate next step?
A) Reduce the dose of Enalapril
B) Hemodialysis
C) Insulin Intravenous
D) Calcium Gluconate IV
E) Sodium biacrbonate IV
Filed under: Uncategorized, USMLE Test Prep | Tagged: ARCHER ACID-BASE, Archer cardiology, ARCHER ELECTROCARDIOGRAMS, ARCHER FLUID AND ELECTROLYTES, ARCHER NEPHROLOGY, dr.red nephrology lecture, USMLE ELECTROCARDIOGRAMS, USMLE STEP 3 CARDIOLOGY, usmle step 3 nephrology | 11 Comments »
Posted on January 26, 2012 by Archer USMLE Reviews
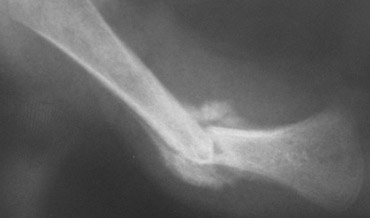
313) A 54 year old man is evaluated in your office for swelling of bilateral wrists and ankles. He also describes pain in his wrists and ankles as well as in the lower legs. Symptoms started 2 months ago and have been progressively worse. He reports limitation in walking because of extreme pain. He denies any stiffness. His past medical history is significant for chronic obstructive pulmonary disease for which he uses Tiotropium inhaler. He recently quit smoking but reports having smoked about 2 packs per day for 35 years. On physical examination, his vitals are within normal limits. Musculoskeletal exam reveals swelling and tenderness in bilateral wrists and ankles. There is an associated grade 3 clubbing in the fingers. There also tenderness all over the tibiae. Overlying skin is thickened and erythematous. An erythrocyte sedimentation rate is elevated at 30 mm/hr. An x-ray of his upper extremity is shown below:

Which of the following investigations should be ordered next?
A) Arterial Doppler
B) Rheumatoid Factor
C) Hepatitis C serology
D) CT Scan of the Chest
E) Anti-Citrullin Peptide
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer pulmonology, Archer Rheumatology, arthritis, USMLE STEP 3 PULMONOLOGY, USMLE step 3 Rheumatology | 6 Comments »
Posted on January 25, 2012 by Archer USMLE Reviews
312) A 73 year old man with history of Dementia and well-controlled Parkinson’s disease was admitted to the hospital 3 days ago with fever, hypotension and dysuria. He was diagnosed with sepsis secondary to urinary tract infection and has been on treatment with Ampicillin and Gentamicin. Urine cultures revealed enterococci. Over the past two days, his blood pressure improved and he has been afebrile however, he has become increasingly immobile and excessively tremulous. He is unable to rise from a chair or walk without help. His home medications include Levodopa, Benserazide and Selegeline. On physical examination, blood pressure is 130/80 mm Hg. He is alert, awake and oriented. He has severe bilateral resting tremor, generalized rigidity and bradykinesia . Results of routine blood tests showed no abnormality and CT of the head is normal. Which of the following is the most appropriate management at this time?
A) Increase Levodopa
B) Add Carbidopa
C) Discontinue Gentamicin
D) Add Piperacillin-Tazobactam
E) Start Bromocriptine
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer Infectious Diseases, archer neurology, neurology mcq, neurology usmle mcqs, USMLE STEP 3 INFECTIOUS DISEASES, usmle step 3 neurology | 6 Comments »
Posted on January 17, 2012 by Archer USMLE Reviews
311) A 3 year old male child is brought to the emergency room by his mother after he fell from his tricycle and sustained an injury to his head . The child was found to be alert and awake after the fall, however, he reported mild pain on the right side of his head. His mother noted a small bruise and swelling over the right side of his scalp. There is no history of vomiting or nausea. He has no past history of convulsions or epilepsy. Family history is unremarkable. At this time, child is quiet and reports mild headache. On examination, he is alert and awake. He is not in distress. There is small contusion on the fronto-parietal aspect of his scalp. There is no evidence of hematoma. Palpation does not reveal any depressed fracture. Neurological examination is normal with out any deficits. Rest of the physical exam is normal. Which of the following is the most appropriate management at this time?
A) Contact Child Protection Services
B) Perform Head CT scan
C) Admit to Hospital
D) Observe at home
E) Skull X-rays
Filed under: Uncategorized, USMLE Test Prep | Tagged: archer neurology, archer pediatrics, emergency medicine archer, neurology usmle mcqs, usmle step 3 emergency medicine, usmle step 3 neurology, USMLE STEP3 PEDIATRICS | 13 Comments »
Posted on January 17, 2012 by Archer USMLE Reviews
310) A 28 year old man is admitted with abdominal pain and diarrhea of one day duration. Abdominal pain is diffuse in nature, mild to moderate and is associated with cramps and vomiting. He reports having had recurrent attacks of abdominal pain and diarrhea for several months. His past medical history is significant for Vitiligo and Hypothyroidism. He denies any allergies, atopy or Asthma. Family history is unremarkable. On examination, his mucous membranes and dry and he appears moderately dehydrated. He is afebrile, Blood pressure is 90/60 mm HG, heart rate 120/min, Respiratory rate 18/min. There is no peripheral lymphadenopathy. Skin examination reveals hypopigmented patches consistent with Vitiligo on his chest and the extremities. Abdominal examination is benign , Spleen is not palpable. CT scan of the chest, abdomen and pelvis are normal. Stool anlaysis performed several times during his previous episodes did not reveal any evidence of parasitic infection or leukocytes or blood. Laboratory investigations and peripheral smear are shown below:
 WBC 6.0k/µl
WBC 6.0k/µl
Differential: Neutrophils 45%, Lymphocytes 34% ( N = 20 to 40%), Monocytes 6%, Eosinophils 15% ( normal range 1 to 4%)
Hemoglobin 14.5 g/dL ( Normal = 13.0 to 16.5 gm%),
Mean cell volume (MCV) 84 fL
Platelet count 310k/µl
Stool Ova and Parasites negative
TSH 4 μIU/ml ( 0.3 – 5.0 uIU/ml)
Which of the following diagnoses is most likely explanation for the patient’s clinical presenation?
A) Giardiasis
B) Addison’s disease
C) Vitiligo
D) Chronic Myeloid Leukemia
E) Lymphoma
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer hematology, Hematology, USMLE step 3 Hematology | 33 Comments »
Posted on January 9, 2012 by Archer USMLE Reviews
309) A 76-year-old man presented with a 4-month history of recurrent vertigo. He reports feeling a sensation of spinning dizziness on turning the neck to his left. He also reports left sided headaches and decreased hearing on the left. Each episode lasted about 15 to 20 minutes and occurred when he turned his head to the left. He denies any ringing sensation in ears, nausea or vomiting. He denies any chest-pain, shortness of breath or palpitations. His past medical history is significant for hypertension and diet controlled diabetes. His medications include hydrochlorothiazide and enalapril. He also has history chronic neck pain due to cervical spondylosis for which he uses tylenol. On examination, his blood pressure in supine position is 140/88 mmHg and blood pressure on standing is is 130/86. Tympanic membranes are visible and there is some cerumen in the left ear. Using a 512Hz tuning fork , bone conduction is found to be better than air conduction on the left and Weber test shows lateralization to the left. Dix-Hallpike’s and Lhermitte’s signs are negative. There are no other neurological deficits. Gait is normal. Range of motion of the neck is limited on lateral movements and neck pain is elicited by turning to left side. An X-ray of cervical spine shows severe spondylosis with discopathy and osteophytes from C2 to C4 vertebrae. Which of the following is the most appropriate management of his dizziness?
A) Discontinue Hydrochlorthiazide
B) Cervical Collar
C) Cerumen Disimpaction
D) Increase Diuretics and add Meclizine
E) Methylprednisolone
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer ENT, archer neurology, neurology mcqs, neurology usmle mcqs, USMLE STEP 3 ENT, usmle step 3 neurology, vertigo | 7 Comments »
Posted on January 9, 2012 by Archer USMLE Reviews
308) A 76-year-old man presented with a 4-month history of recurrent vertigo. He reports feeling a sensation of spinning dizziness on turning the neck to his left. He also reports left sided headaches and decreased hearing on the left. Each episode lasted about 15 to 20 minutes and occurred when he turned his head to the left. He denies any ringing sensation in ears, nausea or vomiting. He denies any chest-pain, shortness of breath or palpitations. His past medical history is significant for hypertension and diet controlled diabetes. His medications include hydrochlorothiazide and enalapril. He also has history chronic neck pain due to cervical spondylosis for which he uses tylenol. On examination, his blood pressure in supine position is 140/88 mmHg and blood pressure on standing is is 130/86. Tympanic membranes are visible and there is some cerumen in the left ear. Using a 512Hz tuning fork , bone conduction is found to be better than air conduction on the left and Weber test shows lateralization to the left. Dix-Hallpike’s and Lhermitte’s signs are negative. There are no other neurological deficits. Gait is normal. Range of motion of the neck is limited on lateral movements and neck pain is elicited by turning to left side. An X-ray of cervical spine shows severe spondylosis with discopathy and osteophytes from C2 to C4 vertebrae. Which of the following is the most likely explanation for his Vertigo?
A) Orthostatic Hypotension
B) Vertebral artery occlusion from cervical spondylosis
C) Cerumen Impaction
D) Meniere’s disease
E) Labyrinthitis
Filed under: Uncategorized, USMLE Test Prep | Tagged: archer neurology, archer obstetrics, archer ostetrics and gynecology, archer preventive medicine, neurology mcqs, neurology usmle mcqs, usmle step 3 gynecology and obstetrics, usmle step 3 neurology, usmle step 3 obstetrics, usmle step 3 preventive medicine, vaccinations usmle step 3, vertigo | 7 Comments »
Posted on January 6, 2012 by Archer USMLE Reviews
307) A 35 year old woman is evaluated in your office during an antenatal visit. Her last menstrual period was 8 weeks ago. She tells you that 2 weeks after she missed her regular menstrual period she checked herself with home pregnancy kit and tested positive. She works in a day-care center. She is concerned now because she received Rubella vaccination 4 weeks ago after an exposure to a sick child without knowing that she was pregnant. She read about the dangers to fetus on the internet and is very worried. Physical examination is benign.
Which of the following is the most appropriate course of action?
A. Refer her to medical termination of pregnancy
B. Tell her that there is a high established risk to fetus and she should strongly consider termination of pregnancy
C. Counsel her about theoretical risk to fetus and continue pregnancy care
D. Administer Rubella immunoglobulin
E. Reassure her that there is no risk to fetus.
Filed under: Uncategorized, USMLE Test Prep | Tagged: archer obstetrics, archer ostetrics and gynecology, archer preventive medicine, usmle step 3 gynecology and obstetrics, usmle step 3 obstetrics, usmle step 3 preventive medicine, vaccinations usmle step 3 | 6 Comments »
Posted on January 6, 2012 by Archer USMLE Reviews
306) A 32 year old man with history of immune thrombocytopenic purpura is evaluated in your office during a follow up visit. His previous treatments include intravenous immunoglobulin (IVIG) and steroids for his immune thrombocytopenia. He has responded to IVIG in the past however, the response was transient despite steroid maintenance. The patient was maintained on steroids for 2 months initially and achieved a sub-optimal response with peak platelet count reaching 30k/µl. He began very slow steroid taper over the last 4 weeks but his platelets have dropped to 8k/μl again during the taper. Hence, the patient is scheduled for Splenectomy. On examination, he has no bleeding or echymoses. Platelet count today is 10k/μl. Which of the following is the most appropriate step in preparing this patient for surgery?
A) Pneumococcal , Meningococcal and HIB vaccines 1 week prior to surgery
B) Pneumococcal and meningococcal vaccines 2 weeks prior to surgery
C) Pneumococcal, Menigococcal and HIB vaccines 2 weeks prior to surgery
D) Daily oral Penicillin Prophylaxis
E) No vaccines required in adults
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer hematology, archer preventive medicine, archer surgery, USMLE step 3 Hematology, usmle step 3 preventive medicine, usmle step 3 surgery | 11 Comments »
Posted on January 5, 2012 by Archer USMLE Reviews
305) You have recently been posted by your employer to serve as a school physician in a school that is few miles away from your office. The school has about 250 students of whom 55% are girls and the rest are boys. The school teacher reports that they have not had a scoliosis screening program in place and wonders if you can implement such a program in the school. Which of the following is the most appropriate course of action?
A) Arrange scoliosis screening for all students between 10 and 16 years of age.
B) Arrange scoliosis screening for all students 10, 12, 14 and 16 years of age.
C) Contact the school nurse and review skills for scoliosis screening procedures.
D) Visually inspect for severe curves only when the back is examined for other reasons.
E) Screen girls for scoliosis at 15 years of age and boys at 16 years of age.
Filed under: Uncategorized, USMLE Test Prep | Tagged: aRCHER ORTHOPEDICS, archer pediatrics, archer preventive medicine, school nurse, school physician, scoliosis, scoliosis screening, screening procedures, USMLE STEP 3 ORTHOPEDICS, usmle step 3 preventive medicine, USMLE STEP3 PEDIATRICS | 5 Comments »
Posted on January 5, 2012 by Archer USMLE Reviews
304)
A 16-year-old male who presents to your office for his regular health checkup and for clearance before participation in then high school basketball team. During the physical examination, you note a mild convexity in the thoracic region of his spine with forward flexion at the hips. You ask him to lean forward with his feet together and bend 90 degrees at the waist. Based on your clinical examination, you estimate a lateral spinal curvature of about 5 degrees. You discuss these findings with the patient and his mother. Which of the following is the most appropriate action?
A. Recommend back-strengthening exercises.
B. Refuse medical clearance for participation in sports.
C. Order a radiograph of the back to quantify the curvature
D. Observation alone.
E. Refer for orthopedic consultation.
Filed under: Uncategorized, USMLE Test Prep | Tagged: aRCHER ORTHOPEDICS, archer pediatrics, archer preventive medicine, USMLE STEP 3 ORTHOPEDICS, usmle step 3 preventive medicine, USMLE STEP3 PEDIATRICS | 8 Comments »
Posted on January 4, 2012 by Archer USMLE Reviews
303) A 11 year old girl is evaluated in your office for progressing lateral curvature of her spine. She denies any back pain or neurological symptoms. Her mother is very concerned about the child’s appearance. On physical examination, there is gross convexity in the thoracic region of her spine with forward flexion at the hips. There is no tenderness or neurological deficits. An x-ray of the spine reveals 25º curvature ( cob angle) . Which of the following is the most appropriate management at this time?
A) Repeat Clinical exam and x-rays at 6 months
B) Refer to orthopedic evaluation
C) Bracing
D) Spinal fusion surgery
E) Recommend back strengthening exercises
Filed under: Uncategorized, USMLE Test Prep | Tagged: aRCHER ORTHOPEDICS, archer pediatrics, USMLE STEP 3 ORTHOPEDICS, USMLE STEP3 PEDIATRICS | 5 Comments »
Posted on January 4, 2012 by Archer USMLE Reviews
302) A 16 year old girl is evaluated in your office for one day duration of fever, cough and left pleuritic chest pain. On examination, her temperature is 100.5F, respiratory rate is 18/min, pulse 100/min and blood pressure 120/60 mm hg. Breath sounds are decreased in the left lower lobe. A Chest x-ray is obtained which reveals left lower lobe infiltrate. Incidentally, a 7 ° lateral curvature is seen on the chest x-ray. The patient is started oral azithromycin for her pneumonia and is discharged home. Which of the following is the most appropriate management for her incidentally discovered scoliosis?
A) Clinical follow up alone
B) Repeat x-rays every 6 months
C) Refer to orthopedic surgery
D) Bracing
E) No follow up required
Filed under: Uncategorized, USMLE Test Prep | Tagged: aRCHER ORTHOPEDICS, archer pediatrics, USMLE STEP 3 ORTHOPEDICS, USMLE STEP3 PEDIATRICS | 11 Comments »
Posted on January 4, 2012 by Archer USMLE Reviews
301) A five month old male infant is brought to the out patient department for evaluation of one month history of recurrent vomiting, diarrhea and skin rash . The baby was delivered normally at term with out any complications. Mother reports that she breastfed him for four months and recently has been feeding him exclusively with formula. Mother reports that the baby vomits intermittently after each feed and develops raised, red welts on his skin after each feeding. There is no blood or bile in the vomitus. Vomiting occurs within 30 minutes after feeding. Suckling is normal. He also has mucousy, loose stools for the past three weeks with no blood. There is no history of cough, cold or fever. On examination, the infant in no apparent distress and vitals are normal. Abdominal examination is benign with out any palpable masses or peristaltic waves. Rest of the physical is normal. Laboratory investigations reveal Hb: 13.2 gm%; Haematocrit: 35%; WBC: 9,200/μl ; Platelets: 225,000/μl, Na 132 meq/L; K 3.8 meq/L; Cl 92 meq/L; albumin 4.6g%. Urinalysis is normal. Which of the following is the most appropriate next step in managing this condition?
A) Abdominal ultrasound
B) Lactose free formula
C) Start hydrolyzed formula feeds
D) IgE Radio-allergosorbent test
E) Observation
Filed under: Uncategorized, USMLE Test Prep | Tagged: ARCHER GASTROENTEROLOGY, archer pediatrics, USMLE STEP 3 GASTROENEROLOGY, USMLE STEP3 PEDIATRICS | 19 Comments »
Posted on January 4, 2012 by Archer USMLE Reviews
300) A 14 year old girl is evaluated in your office for moderate headache of one month duration . She denies any blurred vision, neck stiffness or fever. She is accompanied by her mother who reports that her performance at school has progressively declined over the last few months and she has deepening of voice for the past 4 months. On examination, Pulse 80/min; Temperature: 98.4F and Blood pressure: 135/100 mm of Hg. There is excessive hair on her face. Rest of the physical is normal except for faint purplish marks on her abdomen. Laboratory investigations including complete blood count, comprehensive metabolic panel and Urine analysis are within normal limit. Which of the following is the most appropriate next step ?
A) 24 hour urinary cortisol
B) MRI brain
C) CT scan of the abdomen
D) Dexamethasone Suppression Test
E) Plasma catecholamines
F) Urine Drug Screen
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer endocrinology, archer pediatrics, endocrinology questions, usmle step 3 endocrinology, USMLE STEP3 PEDIATRICS | 21 Comments »
Posted on January 4, 2012 by Archer USMLE Reviews
299) A 10 month old male infant is brought by his concerned mother to the Emergency room with complaints of vomiting and bloody diarrhea. Mother reports that he suffered from “stomach flu” symptoms about 1 week ago which resolved spontaneously. He had 4 episodes of vomiting since yesterday and has been crying intermittently every 15 minutes. There is no blood or bile in the vomitus. He had four loose stools with blood in it. There is no history of fever or cough or cold. His past medical history is unremarkable. On examination, temperature is 98.4F, pulse 112, respiratory rate 30/min and blood pressure at 80/50 mm hg. Oral mucosa appear moist and skin turgor is adequate. Abdomen is soft with no palpable masses. Bowel sounds are present. Stool guaiac is strongly positive. Stool is sent for cultures and abdominal x-rays are obtained. An x-ray image is shown below:

Which of the following is the most appropriate next step in managing this condition?
A) Abdominal ultrasound
B) Gastrograffin enema
C) Surgery
D) Rectal tube placement
E) Flexible sigmoidoscopy
Filed under: Uncategorized, USMLE Test Prep | Tagged: ARCHER GASTROENTEROLOGY, archer pediatrics, archer surgery, USMLE STEP 3 GASTROENEROLOGY, usmle step 3 surgery, USMLE STEP3 PEDIATRICS | 23 Comments »
Posted on January 2, 2012 by Archer USMLE Reviews
298) A 6 year old boy presents to your office with a limp on the right side. He denies any falls or trauma. Mother reports that the limp has been present for several weeks. She reports that the patient was seen in the Emergency Room when the limp was first observed. X-rays obtained at that time were normal and so, he was discharged. There is no history of fever. He denies any pain. Family history is unremarkable. On examination, he is afebrile . His right lower extremity appears one inch shorter than the left. Upon standing and walking, his pelvis appears to be tilted towards the left. Which of the following is most likely to be abnormal in this condition?
A) External rotation of hip
B) Tibial tuberosity
C) X-ray of the Knee
D) Erythrocyte Sedimentation Rate
E) Internal rotation and abduction of hip
Filed under: Uncategorized, USMLE Test Prep | Tagged: archer pediatrics, child with limp, limping child, USMLE STEP 3 ORTHOPEDICS, USMLE STEP3 PEDIATRICS | 11 Comments »
Posted on January 2, 2012 by Archer USMLE Reviews
297) A 64 year old man is seen in the office for pre-operative evaluation of right inguinal hernia repair. His past medical history is significant for diabetes and recurrent right foot cellulitis. His most recent episode of right foot cellulitis was 2 weeks ago for which he received a 2 week course of oral antibiotics. His surgery is scheduled within one week. On examination, he is afebrile. He has reducible right inguinal hernia and bilateral lower extremity stasis dermatitis. His laboratory investigations reveal:
Platelet Count 240k/μl ( Normal 150–400k/μl)
Prothrombin time 22 seconds ( Normal 10 to 13 secs)
Partial Thromboplastin time : 34 sec ( Normal 22 to 37 secs)
Which of the following is the most appropriate action at this time?
A) Obtain PTT mixing studies
B) Administer Oral Vitamin K
C) Intravenous Fresh Frozen Plasma
D) Intravenous Factor VIII
E) Von Willebrand Factor Assay
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer hematology, archer surgery, Hematology, USMLE step 3 Hematology, usmle step 3 surgery | 13 Comments »
Posted on December 31, 2011 by Archer USMLE Reviews
The WordPress.com stats helper monkeys prepared a 2011 annual report for this blog.
Here’s an excerpt:
The Louvre Museum has 8.5 million visitors per year. This blog was viewed about 100,000 times in 2011. If it were an exhibit at the Louvre Museum, it would take about 4 days for that many people to see it.
Click here to see the complete report.
Filed under: Uncategorized | Leave a comment »
Posted on December 30, 2011 by Archer USMLE Reviews
296) A 6 month old Asian infant is brought by his concerned aunt for evaluation of dark blue areas on the child’s buttocks. She says she was called to baby-sit the infant since his mother found a new job 2 days ago. She noted the rash and became suspicious that the child may have been abused. The mother arrives in Emergency room an hour later and reports that the rash has been present since birth. The mother is divorced and lives alone with the child. On examination, there are bluish-green patches on bilateral buttocks and on the lower back. They are irregular in shape and margins are indistinct. There is no swelling or tenderness. An image of the skin findings is shown below:

Which of the following is the most appropriate next step ?
A) Order Skeletal Survey
B) Reassure that rash may fade away in few years
C) Contact Child Protection services
D) Obtain Coagulation parameters
E) Obtain Platelet count
Filed under: Uncategorized, USMLE Test Prep | Tagged: archer dermatology, archer pediatrics, dermatology usmle, dermatology usmle step 3 questions, USMLE STEP 3 DERMATOLOGY, usmle step 3 dermatology images, USMLE STEP3 PEDIATRICS | 10 Comments »
Posted on December 30, 2011 by Archer USMLE Reviews
295) A 10 year old boy is brought to your office for evaluation of rash in bilateral axillae and groin for the past 2 months. He denies any itching or any other skin rashes. However, he reports that the area has become progressively rough to touch. He is otherwise, healthy. On examination, there are reddish brown patches in bilateral axillae and groin. There is maceration and scaling in the web spaces between the toes of bilateral feet. Rest of the examination is normal. A KOH mount is obtained and is negative. Wood’s lamp examination reveals coral red fluorescence. A picture of the rash is shown below:

Which of the following is the most appropriate next step ?
A) Topical corticosteroid
B) Topical Selenium Sulfide
C) Oral erythromycin
D) Topical Clotrimazole
E) Oral Metronidazole
Filed under: Uncategorized, USMLE Test Prep | Tagged: archer dermatology, archer pediatrics, dermatology usmle, dermatology usmle step 3 questions, USMLE STEP 3 DERMATOLOGY, usmle step 3 dermatology images, USMLE STEP3 PEDIATRICS | 7 Comments »
Posted on December 30, 2011 by Archer USMLE Reviews
294) A 71 year old woman presents to the emergency room with complaints of bright red bleeding per rectum. She denies any abdominal pain, nausea or vomiting. She has a history of paroxysmal atrial fibrillation. Her medications include aspirin and beta blocker. About 10 days ago, she had a screening colonoscopy. She had a 3cm polyp in the sigmoid colon which was removed at that time. She reports that she did not experience any bleeding immediately after polyp removal and is concerned about this episode that occured so many days after the procedure. On physical examination she is afebrile . Abdominal examination is benign. Rectal examination reveals bright red blood and no palpable hemorrhoids. Patient is anxious about her diagnosis. Which of the following is the most appropriate statement?
A) ” Your bleeding is mostly secondary to ischemic colitis”
B) ” Bleeding can occur up to two weeks after polypectomy”.
C) ” Your bleeding is related to Aspirin use”.
D) ” We will have to repeat colonoscopy to confirm that a cancer has not been missed”
E) ” You will need diagnostic laporoscopy to evaluate the cause”
Filed under: Uncategorized, USMLE Test Prep | Tagged: ARCHER GASTROENTEROLOGY, archer surgery, post-polypectomy bleeding, post-polypectomy complications, post-polypectomy electrocoagulation syndrome, post-polypectomy perforation, USMLE STEP 3 GASTROENEROLOGY, usmle step 3 surgery | 8 Comments »
Posted on December 30, 2011 by Archer USMLE Reviews
293) A 70 year old man is evaluated in the emergency room for abdominal pain , fever, nausea and vomiting that began 8 hours after he underwent a screening colonoscopy. The pain is severe and is mostly in the left lower quadrant of the abdomen. He reports that his colonoscopy procedure was uneventful except that he had a 2cm sessile polyp which was removed during the procedure. He denies any rectal bleeding. On examination, temperature is 102 F, blood pressure 100/60 mmHg, pulse 120, respiratory rate 28/min. Abdominal examination reveals severe tenderness, guarding and rigidity in the left lower quadrant. Laboratory investigations show:
WBC 28k/µl with left shift
Hemoglobin 13.5 g/dL
Mean cell volume (MCV) 84 fL
Platelet count 310k/µl
Which of the following is most important next step in management?
A) Obtain urgent surgical consult
B) Rectal tube placement
C) Serum amylase level
D) Supportive care alone
E) Barium enema
Filed under: Uncategorized, USMLE Test Prep | Tagged: ARCHER GASTROENTEROLOGY, archer surgery, post-polypectomy bleeding, post-polypectomy complications, post-polypectomy electrocoagulation syndrome, post-polypectomy perforation, USMLE STEP 3 GASTROENEROLOGY, usmle step 3 surgery | 10 Comments »
Posted on December 30, 2011 by Archer USMLE Reviews
292) A 66 year old man is evaluated in the emergency room for abdominal pain and fever. The patient underwent a screening colonoscopy in the outpatient Gastroenterology clinic 8 hours ago and had a 3cm sessile polyp removed. He complains of moderate pain in left lower quadrant that started one hour ago. He denies nausea or vomiting or rectal bleeding. On examination, temperature is 100.8F, blood pressure 140/90 mmHg, pulse 102, respiratory rate 20 bpm. Abdominal examination reveals tenderness and guarding in the left lower quadrant. There is no rigidity or rebound tenderness. His laboratory investigations including complete blood count and comprehensive metabolic panel are within normal limits. Which of the following is the most appropriate next step in managing this patient?
A) Exploratory Laporotomy
B) Rectal tube placement
C) Flexible sigmoidoscopy
D) CT Scan of the Abdomen
E) Conservative management
Filed under: Uncategorized, USMLE Test Prep | Tagged: ARCHER GASTROENTEROLOGY, archer surgery, post-polypectomy bleeding, post-polypectomy complications, post-polypectomy electrocoagulation syndrome, post-polypectomy perforation, USMLE STEP 3 GASTROENEROLOGY, usmle step 3 surgery | 10 Comments »
Posted on December 28, 2011 by Archer USMLE Reviews
291) A 66 year old man with past medical history of hypertension and type-2 diabetes mellitus is evaluated in your office during a regular follow up visit for his diabetes. During this visit, he reports problem getting and maintaining an erection. On the times that he does have an erection, they are very soft. He says this problem began approximately 10 months ago and has slowly worsened but he was too embarrassed to disclose this during his previous visits. He still has a strong sexual desire and this problem has caused strain in his current relationship. He is physically very active walking two to three miles per day. His medications include glipizide and hydrocholrthiazide. He says his home blood sugars have been “perfect”. A Hemoglobin A1C 2 weeks ago was 6.0gm% . He currently does not smoke after having quit smoking 15 years ago. Physical examination shows blood pressure 140/90 mmHg, pulse 86, respiratory rate 20 bpm. Genitilia and testicles are normal in size . Peripheral pulses are normal. Rest of the physical examination is normal. Which of the following is the most appropriate next step in managing this patient?
A) Obtain Serum Total Testosterone
B) Obtain Nocturnal Penile Tumescence
C) Start Sildenafil
D) Prescribe Vacuum assisted erection device
E) Switch Hydrochlorthiazide to ACE inhibitor
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer endocrinology, ARCHER UROLOGY, erectile dysfunction, internal medicine board review, male sexual dysfunction, usmle step 3 endocrinology, usmle step 3 urology | 13 Comments »
Posted on December 28, 2011 by Archer USMLE Reviews
290) A 72 year old man with history of Diabetes Mellitus and peripheral vascular disease is evaluated in your office for impotence. He denies any premature ejaculation and states that he can not even attain an erection. Further studies confirm erectlie dysfunction secondary to organic causes. The patient denies any history of angina in the past. His medications include Aspirin, Clopidogrel, Glargine insulin and Lispro. His most recent HGBA1C was 6.5%. You offer him sildenafil for erectlie dysfunction. He is now concerned about the possible side effects. Which of the following is the most common side effect of sildenafil?
A) Headache
B) Nasal congestion
C) Diarrhea
D) Blurred vision
E) Flu like symptoms
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer endocrinology, ARCHER UROLOGY, erectile dysfunction, internal medicine board review, usmle step 3 endocrinology, usmle step 3 urology | 4 Comments »
Posted on December 28, 2011 by Archer USMLE Reviews
289) A 32 year old male athlete is evaluated in the office for bilateral breast enlargement. He is a state champion in running and is scheduled to participate in the national level running championship in few weeks. He is very concerned about his appearance. He denies using any illicit drugs or exogenous androgens or aromatase inhibitors is seen in the office during a routine follow up visit. His past medical history is unremarkable. Physical examination reveals gynecomastia bilaterally. His laboratory investigations reveal:
WBC 8.8k/µl
Hemoglobin 18.5 g/dL ( Normal = 13.0 to 16.5 gm%),
Mean cell volume (MCV) 84 fL
Platelet count 310k/µl
Which of the following is most useful in establishing the diagnosis?
A) Erythropoetin level
B) Urine Drug Screen
C) Serum Total Testosterone
D) Urine Testosterone/ Epitestosterone ratio
E) Serum Free Testosterone
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer endocrinology, archer sports medicine, ARCHER UROLOGY, internal medicine board review, serum testosterone, usmle step 3 endocrinology, usmle step 3 sports medicine, usmle step 3 urology | 12 Comments »
Posted on December 28, 2011 by Archer USMLE Reviews
288) A 38 year old caucasian man is seen in the office during a routine follow up visit. His past medical history is significant for testicular non-seminomatous germ cell tumor diagnosed 9 months ago and was treated with radical orchiectomy of left testicle and chemotherapy. He completed chemotherapy 6 months ago and achieved a complete response. His tumor markers and imaging studies 3 months after completion of therapy were normal. He complains of decreased sexual drive and energy. He denies smoking tobacco or alcohol. He uses Marijuana on a daily basis but quit 2 months ago. His family history is unremarkable. Physical examination shows absent left testicle. Rest of the physical is normal. Serum alpha-fetoprotein is normal. Beta HCG is elevated at 15U/L ( Normal < 5 U/L) . A chest X-ray , CT scan of the abdomen and pelvis are normal. His routine laboratory investigations including complete blood count are within normal limits. Which of the following is most likely reason for his elevated Beta-HCG?
A) Recurrent tumor
B) Marijuana Use
C) Hypogonadism
D) Chemotherapy effect
E) Hyperthyroidism
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer endocrinology, Archer oncology, ARCHER UROLOGY, internal medicine board review, serum testosterone, STEP 3 ONCOLOGY, usmle step 3 endocrinology, USMLE STEP 3 ONCOLOGY, usmle step 3 urology | 10 Comments »
Posted on December 28, 2011 by Archer USMLE Reviews
287) A 38 year old caucasian man is seen in the office due to decreased libido and energy. His past medical history is significant for testicular cancer diagnosed 1 year ago and was treated with radical orchiectomy of left testicle and chemotherapy. He denies smoking tobacco but admits using Marijuana on a daily basis for the past few months. His family history is unremarkable. Physical examination reveals gynecomastia and absent left testicle. Body mass index is 24. His routine laboratory investigations including complete blood count are within normal limits. Serum total testosterone level is reduced and Serum LH concentration is elevated. The patient is started on Testosterone replacement therapy with a testosterone skin gel. Which of the following is the most appropriate step in follow up care of this patient after starting testosterone therapy?
A) Digital Rectal exam and Serum PSA level at one year
B) Hematocrit at 6 months and then, every year
C) DEXA scan at one year
D) Serum Testosterone level at 6 months
E) Serum LH at one month.
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer endocrinology, ARCHER UROLOGY, internal medicine board review, serum testosterone, usmle step 3 endocrinology, usmle step 3 urology | 12 Comments »
Posted on November 27, 2011 by Archer USMLE Reviews
286) A 55 year old woman with history of diabetes mellitus and hypertension is admitted with chest pain. Chest pain started about 30 minutes ago but now resolved after she received sublingual nitroglycerin. An electrocardiogram obtained by EMS showed ST segment depressions but a repeat electrocardiogram in the Emergency room is normal. She is placed on Aspirin, low molecular weight heparin, atorvastatin and metoprolol. She denies any easy bruising, nose bleeding or any other gross bleeding. She denies smoking , alcohol or drug abuse She has not been admitted to any hospital and has never received anticoagulants in the past. Physical examination is benign . Laboratory investigations reveal:
WBC 8.8k/µl
Hemoglobin 15 g/dL,
Mean cell volume (MCV) 84 fL
Platelet count 8k/µl
Liver function tests, Electrolytes, Creatinine, Prothrombin time and Partial thromboplastin time are within normal limits. Three sets of cardiac enzymes are negative. Cardiology team held aspirin and low molecular weight heparin immediately. A peripheral blood smear is shown below:

Which of the following is the most appropriate next step in management?
A) Platelet transfusion
B) Heparin induced platelet antibodies
C) Start Lepirudin
D) Send CBC in a citrate tube
E) IV Gamma Globulin
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer hematology, Hematology, internal medicine board review, USMLE step 3 Hematology | 8 Comments »
Posted on November 27, 2011 by Archer USMLE Reviews
285) A 26 year old man is seen in the office because he was found to have abnormal blood counts during a health check up prior to his life insurance application. He says he was told to see his physicians because his platelet count was very low. He denies any easy bruising, nose bleeding or any other gross bleeding. He has no other medical problems. He denies smoking , alcohol or drug abuse. He denies any recent infections. He leads a very active lifestyle and is a professional soccer player. He proudly states that he won his team the state level championship a year ago and likes to aggressively pursue this career. Physical examination is benign. There is no splenomegaly. Repeat aboratory investigations reveal:
WBC 8.8k/µl
Hemoglobin 15 g/dL,
Mean cell volume (MCV) 84 fL
Platelet count 45k/µl
Liver function tests, Electrolytes, Creatinine, Prothrombin time and Partial thromboplastin time are within normal limits. A peripheral blood smear shows reduced number of platelets with out any schistocytes or blasts or nucleated red cells. Antinuclear antibodies, HIV testing and Hepatitis C are negative.
Which of the following is the most appropriate next step in managing this patient?
A) Intavenous Immunoglobulin
B) Recommend against soccer for life
C) Splenectomy
D) Observation
E) Prednisone
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer hematology, Hematology, internal medicine board review, USMLE step 3 Hematology | 10 Comments »
Posted on November 27, 2011 by Archer USMLE Reviews
284) A 32 year old pregnant woman is evaluated in the emergency room for new onset abdominal pain. She has mild nausea and vomited once prior to arrival in the emergency room. She denies any bleeding . This is her first pregnancy and she is at 34 weeks gestation. Physical examination reveals normal blood pressure. There is mild tenderness in epigastric region. Laboratory investigations reveal:
WBC 10k/µl
Hemoglobin 7 g/dL,
Mean cell volume (MCV) 84 fL
Platelet count 50k/µl
Lactic Dehydrogenase 1200U/L
AST 120U/L
ALT 180U/L
Serum Electrolytes, Creatinine, Prothrombin time and Partial thromboplastin time are within normal limits. Amylase and lipase are normal. A peripheral blood smear shows reduced number of platelets and some fragmented red blood cells. Antinuclear antibodies, Anti-phospholipid antibodies, Lupus anticoagulant profile, HIV testing and Hepatitis C are negative.
Which of the following is the most appropriate next step in management?
A) Platelet transfusion
B) Intravenous Methyl Prednisolone
C) Induction of labor
D) Observation
E) Plasmapheresis
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer hematology, archer obstetrics, Hematology, internal medicine board review, obstetrics, usmle step 3 gynecology and obstetrics, USMLE step 3 Hematology, usmle step 3 obstetrics | 8 Comments »
Posted on November 27, 2011 by Archer USMLE Reviews
283) A 26 year old man is seen in the office during a pre-employment health check-up. He has no medical problems. He denies smoking , alcohol or drug abuse. Physical examination is benign. Laboratory investigations reveal:
WBC 8.8k/µl
Hemoglobin 15 g/dL,
Mean cell volume (MCV) 84 fL
Platelet count 45k/µl
Liver function tests, Electrolytes, Creatinine, Prothrombin time and Partial thromboplastin time are within normal limits. A peripheral blood smear shows reduced number of platelets with out any schistocytes or blasts or nucleated red cells. Antinuclear antibodies, HIV testing and Hepatitis C are negative.Upon further questioning, he denies any easy bruising, nose bleeds or gross bleeding. There is no family history of thrombocytopenia or bleeding disorder.
Which of the following is the most appropriate next step in managing this patient?
A) Intavenous Immunoglobulin
B) Prednisone
C) Observation
D) Bone marrow biopsy
E) Platelet transfusion
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer hematology, Hematology, internal medicine board review, USMLE step 3 Hematology | 5 Comments »
Posted on November 27, 2011 by Archer USMLE Reviews
282) A 32 year old woman is seen in the antenatal clinic during her regular antenatal visit. This is her first pregnancy and she is at 32 weeks gestation. She takes prenatal vitamins. She currently has no complaints. Physical examination is benign. Laboratory investigations reveal:
WBC 10k/µl
Hemoglobin 14 g/dL,
Mean cell volume (MCV) 84 fL
Platelet count 70k/µl
Liver function tests, Electrolytes, Creatinine, Prothrombin time and Partial thromboplastin time are within normal limits. A peripheral blood smear shows reduced number of platelets with out any schistocytes or blasts or nucleated red cells. Antinuclear antibodies, HIV testing and Hepatitis C are negative. The patient is concerned about her abnormal platelet counts. She denies any easy bruising or nose bleeds or gross bleeding. Her complete blood count 3 months ago was completely normal.
Which of the following is the most appropriate response?
A) “You will require treatment with steroids”
B) “Urgent delivery with cesarean section is required.”
C) “Your platelet count will normalize within 2 to 12 weeks after delivery”
D) “You will require Bone marrow biopsy”
E) “No treatment needed since it is immune thrombocytopenia”
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer hematology, archer obstetrics, Hematology, internal medicine board review, obstetrics, usmle step 3 gynecology and obstetrics, USMLE step 3 Hematology, usmle step 3 obstetrics | 5 Comments »
Posted on November 27, 2011 by Archer USMLE Reviews
281) A 22 year old woman is seen in the office for a rash on legs. She had an upper respiratory tract infection one week ago which resolved spontaneously. She is not on any medications. She has no other significant mast medical history. She has easy bruising which started 5 days ago but denies any nose bleeds or gross bleeding. Her last menstrual period was one week ago and she has regular cycles with no history of menorrhagia. Family history is negative for any bleeding disorders or thrombocytopenia. She denies any smoking , alcohol or drug abuse. Physical examination is benign except for petechiae on her bilateral lower extremities. There is no splenomegaly on examination. Laboratory investigations reveal:
WBC 10k/µl
Hemoglobin 14 g/dL,
Mean cell volume (MCV) 84 fL
Platelet count 18k/µl
Liver function tests, Electrolytes, Creatinine, Prothrombin time and Partial thromboplastin time are within normal limits. A peripheral blood smear shows reduced number of platelets with out any schistocytes or blasts or nucleated red cells. Antinuclear antibodies, HIV testing and Hepatitis C are negative.
Which of the following is the most appropriate next step in managing this patient?
A) Ristocetin cofactor assay
B) Prednisone
C) Observation
D) Bone marrow biopsy
E) Plasmapheresis
F) Platelet transfusion
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer hematology, Hematology, internal medicine board review, USMLE step 3 Hematology | 8 Comments »
Posted on November 25, 2011 by Archer USMLE Reviews
280) A 2 year old child is brought by her mother to the emergency department because the child has not been ambulating since yesterday after he tripped over an object and fell. Physical examination reveals tenderness and swelling in left mid-thigh. Eyes are normal without any hemorrhages. Skin reveals several bruises. Teeth are translucent and show yellow discoloration. Moderate scoliosis is evident. A skeletal survey reveals rib fractures and multiple fractures in various stages of healing. There is diffuse osteopenia. There is a spiral fracture of left femur shaft. The limb is splinted and an orthopedic consult is obtained. Which of the following is the most appropriate action?
A) Contact social services
B) Contact Child Protection Services
C) Place the child in foster care
D) Obtain Head CT
E) Obtain detailed family history
Filed under: Uncategorized, USMLE Test Prep | Tagged: aRCHER ORTHOPEDICS, archer pediatrics, USMLE STEP 3 ORTHOPEDICS, USMLE STEP3 PEDIATRICS | 12 Comments »
Posted on November 25, 2011 by Archer USMLE Reviews
279 ) A 14 month-old child is brought by her concerned father to the Emergency department with a history that the child slipped out and fell on the ground from a table that is 10 feet in height. He says the accident occurred last night when he let the child stand on the table. The child cries when the right thigh is touched and does not move the right lower extremity. Rest of the physical examination is normal. There are no suspicious bruises or contusions on the skin. An x-ray of the right femur is shown below.
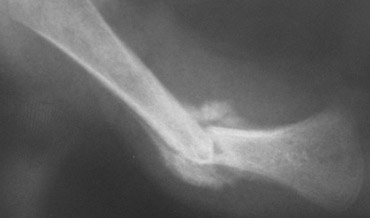
A skeletal survey is obtained and does not show any other fractures. There are no skull fractures or retinal hemorrhages or neurological deficits.
Based on the x-ray findings and the history, which of the following is the most likely diagnosis?
A) Osteogenesis Imperfecta
B) Fibrous Dysplasia
C) Accidental Injury
D) Child Abuse
E) Pathological Fracture from Ewing Sarcoma
Filed under: Uncategorized, USMLE Test Prep | Tagged: aRCHER ORTHOPEDICS, archer pediatrics, USMLE STEP 3 ORTHOPEDICS, USMLE STEP3 PEDIATRICS | 17 Comments »
Posted on November 25, 2011 by Archer USMLE Reviews
278) A 34 year old mother brings her 18 month old child to the emergency room. She is in tears and reports that the child was playing on the sofa and has fallen down 1 day ago landing on his left foot and since then has not been moving his left lower extremity. The child is crying incessantly. Physical examination reveals tenderness and swelling in the left mid-thigh. An x-ray of the left lower extremity shows a non-displaced hair line fracture of the femur shaft and the fracture age consistent with reported history of time of injury. Which of the following is the most appropriate next step in management?
A) Contact Child Protection Services
B) Skeletal Survey
C) Open reduction and internal fixation
D) Bone scan
E) CT head
Filed under: Uncategorized, USMLE Test Prep | Tagged: aRCHER ORTHOPEDICS, archer pediatrics, USMLE STEP 3 ORTHOPEDICS, USMLE STEP3 PEDIATRICS | 7 Comments »
Posted on November 25, 2011 by Archer USMLE Reviews
277) A 32 year old woman with history of Systemic Lupus Erythematosus is evaluated during a routine antenatal visit. Her last menstrual period was 18 weeks ago. She is using prenatal pills and has no complaints. She is being maintained on prednisone. Physical examination is benign and her blood pressure is normal. Her laboratory investigations show positive ANA, Anti-Ds DNA and Anti-SSA (Anti-Ro) antibodies in high titers. Anticardiolipin antibodies and Lupus anticoagulant testing is negative. She is concerned about the risk to her baby because she heard that her antibodies can cross the placenta. Which of the following conditions is most likely to occur in the baby due to passive transfer of maternal antibodies?
A) Lupus Nephritis
B) Aplastic anemia
C) No risk with passive transfer
D) Complete Heart Block
E) Hydrops fetalis
Filed under: Uncategorized, USMLE Test Prep | Tagged: archer obstetrics, archer pediatrics, Archer Rheumatology, neonatology, usmle step 3 obstetrics, USMLE step 3 Rheumatology, USMLE STEP3 PEDIATRICS | 7 Comments »
Posted on November 14, 2011 by Archer USMLE Reviews
276) A 70 year old obese woman is evaluated in your office during an annual follow up visit. Her other medical problems include hypertension, chronic sinusitis, nasal polyps, asthma, osteoarthritis and a history of transient ischemic attack about 2 months ago. She uses acetaminophen for her arthritis pain because ibuprofen makes her “swell up” and causes severe “breathing problems”. Upon review of her medications, you note that she is not on any antiplatelet therapy. Physical examination is unremarkable except for nasal polyps. Which of the following recommendations is most appropriate management for this patient?
A) Warfarin
B) Aspirin and Dipyridamole
C) Aspirin
D) Clopidogrel
E) Dipyridamole
F) No anti-platelet therapy
Filed under: Uncategorized, USMLE Test Prep | Tagged: archer neurology, archer preventive medicine, neurology mcqs, neurology usmle mcqs, stroke prevention, usmle step 3 neurology, usmle step 3 preventive medicine | 5 Comments »
Posted on November 14, 2011 by Archer USMLE Reviews
275) A 70 year old obese woman is evaluated in your office during an annual follow up visit. She has a history of moderate osteoarthritis and she takes over the counter ibuprofen for arthritis pain. She was recently hospitalized with one episode of gastro-intestinal bleeding about 6 months ago. She is being maintained on a proton pump inhibitor. Her other medical problems include hypertension and a history of transient ischemic attack about 2 months ago. Upon review of her medications, you note that she is not on any antiplatelet therapy. Physical examination is unremarkable. Which of the following recommendations is most appropriate management for this patient?
A) Warfarin
B) Aspirin and Dipyridamole
C) Aspirin
D) Clopidogrel
E) Dipyridamole
F) No anti-platelet therapy
Filed under: Uncategorized, USMLE Test Prep | Tagged: archer neurology, archer preventive medicine, neurology mcqs, neurology usmle mcqs, stroke prevention, usmle step 3 neurology, usmle step 3 preventive medicine | 6 Comments »
Posted on November 14, 2011 by Archer USMLE Reviews
274) A 76 year old obese woman with history of uncontrolled Hypertension and Type 2 Diabetes is evaluated in your office during a follow-up visit. She has history of atrial fibrillation and has been taking warfarin for stroke prevention. However, she has difficulty keeping up with her appointments for INR monitoring and does not wish to continue warfarin. Mini mental status examination reveals mild dementia. Get up and Go test does no show any increased risk of fall. She denies any active bleeding. Rest of her physical examination is unremarkable. Her INR is 1.3 and her previous INRs have been sub-therapeutic. Laboratory investigations including complete blood count, serum creatinine and liver function tests are within normal limits. Which of the following management options is most appropriate for this patient?
A) Aspirin alone
B) Aspirin and Dipyridamole
C) Reduced intensity warfarin
D) Low Molecular Weight Heparin
E) Dabigatran
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, Archer hematology, archer preventive medicine, stroke prevention, USMLE STEP 3 CARDIOLOGY, USMLE step 3 Hematology, usmle step 3 preventive medicine | 7 Comments »
Posted on November 14, 2011 by Archer USMLE Reviews
273 ) A 58 year old man with history of chronic smoking and coronary artery disease is seen in your office for a second opinion regarding smoking cessation. He suffered an acute myocardial infarction two years ago and has had percutaneous coronary intervention with stent placement. He has not had any coronary events in the past 2 years. He denies any chest pain. He was recently placed on Nicotine patches for treatment of tobacco use by his primary care physician. The patient is concerned that the nicotine may increase his risk of having a coronary event and requests you for a second opinion regarding nicotine patch therapy. Physical examination is unremarkable. Which of the following is the most appropriate response?
A) Nicotine replacement is contraindicated in patients with cardiovascular diseases
B) Periodic counselling alone is very effective for smoking cessation.
C) Nicotine patch is not an independent risk factor for acute myocardial infarction
D) Your doctor knows what is best for you and you should follow his recommendations.
E) Varenicline is completely safe smoking cessation strategy in patients with cardiovascular disease.
Filed under: Uncategorized, USMLE Test Prep | Tagged: archer preventive medicine, cancer prevention, smoking cessation strategies, usmle step 3 preventive medicine | 5 Comments »
Posted on November 13, 2011 by Archer USMLE Reviews
272 ) A 58 year old man with history of chronic obstructive pulmonary disease and seizure disorder is evaluated in your office during a follow-up visit. He uses tiotropium inhaler on a daily basis and his pulmonary symptoms are adequately controlled. However, he reports inability to comply with smoking cessation recommendations. He has tried counseling sessions and Nicotine replacement therapy in the past without any success. The patient has been counseled again during this visit. Which of the following recommendations is most appropriate for this patient?
A) Nortriptyline
B) Varenicline
C) Bupropion and Telephone Counseling
D) Group therapy
E) Topiramate
Filed under: Uncategorized, USMLE Test Prep | Tagged: archer preventive medicine, cancer prevention, smoking cessation strategies, usmle step 3 preventive medicine | 8 Comments »
Posted on November 13, 2011 by Archer USMLE Reviews
271 ) A 52 year old man is distressed about his inability to quit smoking despite several office-based counseling and telephone counseling sessions. He has tried alternative therapies such as hypnosis and acupuncture without any benefit. His history is significant for severe depression for which he has been on treatment with Fluoxetine. He was recently diagnosed with coronary artery disease and had a stent placed 4 months ago. He understands that his smoking behavior greatly increases his risk of having a coronary event. He says he feels increasingly depressed about his inability to quit smoking. He denies any suicidal ideation. Which of the following is the most appropriate recommendations for this patient?
A) Nicotine replacement therapy
B) Varenicline
C) Buporopion
D) Rimonabant
E) Group therapy
Filed under: Uncategorized, USMLE Test Prep | Tagged: archer preventive medicine, cancer prevention, usmle step 3 preventive medicine | 10 Comments »
Posted on November 13, 2011 by Archer USMLE Reviews
270 ) A 62 year old man presents with complaints of chronic cough for the past two years. Cough occurs mostly in the morning and is associated with mild sputum production. Lately, he has noticed mild shortness of breath on exertion. He denies any chest pain or weightloss. He has a 50 pack year history of smoking. He has been counselled against smoking several times in the past but he believes it is quite difficult for him to quit smoking. He is concerned about lung cancer and requests if he can placed on an annual screening protocol. A chest x-ray and a CT scan of the chest show changes consistent with chronic obstructive pulmonary disease. There is no evidence of malignancy. Which of the following is the most appropriate screening recommendation for this patient?
A) Sputum Cytology every 6 months
B) Chest X-ray annually
C) No Screening
D) Spiral CT scan annually
E) PET scan annually
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer oncology, archer preventive medicine, Archer pulmonology, archer step 3 pulmonology, cancer prevention, STEP 3 ONCOLOGY, USMLE STEP 3 ONCOLOGY, USMLE STEP 3 PULMONOLOGY | 14 Comments »
Posted on November 7, 2011 by Archer USMLE Reviews
269 ) A 42 year old man is evaluated in the Emergency room for sudden onset pain and swelling in the right knee. He denies any trauma. His past medical history is significant for chronic alcohol abuse, diabetes and stage III chronic kidney disease. On physical examination, temperature is 100.5F and heart rate 110. Right knee is grossly swollen, warm, tender and erythematous. Rest of the physical examination is within normal limits. Arthrocentesis is performed and results reveal polymorphonuclear leucocytes of 50,000/µl and intra-cellular negatively birefringent needle shaped crystals under polarized microscopy. Synovial fluid gram stain is negative and bacterial cultures are pending. Complete blood count shows a white blood cell count of 18,000/µl with left shift. Which of the following is the most appropriate management recommendation?
A) Colchicine
B) Indometacin
C) Oral Prednisone
D) Broad spectrum antibiotics
E) Intra-articular Triamcinolone
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer Rheumatology, rhe, USMLE step 3 Rheumatology | 16 Comments »
Posted on November 7, 2011 by Archer USMLE Reviews
268 ) A 62 year old man with history of chronic alcohol abuse, Hepatitis C and gout is admitted for nausea, vomiting and diarrhea. His medications include colchicine for gout prophylaxis and multivitamins. The patient admits that he has increased his alcohol intake to about 4 pints vodka per day over the past two weeks. He has not been drinking or eating adequately. On physical examination, his vitals reveal a heart rate of 110 and blood pressure of 90/60. Oral mucosa are dry with poor skin turgor. Abdominal examination is benign. Laboratory investigations reveal acute renal insufficiency with a creatinine of 4mg% and BUN of 90mg%. His liver functuion tests are elevated with an AST of 160U/L, ALT 70U/L and ALP 240U/L. Total bilirubin is 2.0mg%. Complete blood count shows hemoglobin of 8.6gm%, WBC count of 1.6k/µl with absolute neutrophil count of 500/µl and Platelets 56k/μl. His laboratory investigations three months ago were with in normal limits. CT scan of the abdomen does not show any evidence of liver cirrhosis or Splenomegaly. The patient is started on intravenous hydration, thiamine and folic acid. Which of the following is the most appropriate next step in managing this patient”s pancytopenia?
A) Renal biopsy
B) Liver Biopsy
C) Stop colchicine
D) Bone marrow biopsy
E) Parvo virus RNA
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer hematology, Archer hematology. usmle step 3 hematology, Hematology, USMLE step 3 Hematology | 6 Comments »