Posted on July 8, 2018 by Archer USMLE Reviews
#493. A 77-year-old male is brought into the Emergency Department after the staff at his nursing home witnessed a syncopal event. Once a week a barber comes to the nursing home to provide haircuts and shaving services. After the barber raised the head of the patient’s bed and started to shave his neck, the patient suddenly lost consciousness. The barber called for help, and the patient was regaining consciousness by the time staff arrived. Within a few minutes the patient was at his baseline mental status and did not lose control of his bladder or bowels or bite his tongue during the episode. The barber didn’t notice any abnormal movements by the patient but reports he was trying a new “natural” shaving foam this morning. The patient has a history of Parkinson’s disease and hypertension. He does not smoke or drink alcohol. Blood pressure is 124/84 mm Hg and heart rate is 92 beats/minute sitting and 128/82 mm Hg and 88 beats/minute after standing two minutes. What would be the next best step in management?
A. Immediate referral for permanent pacemaker
B. Carbamazepine
C. Referral to an Electrophysiologist
D. Carotid endarterectomy
E. Reassurance, education and clinical follow-up
cardio@jamesv
Filed under: USMLE STEP III QUESTION BANK, USMLE Test Prep | Tagged: Archer cardiology, cardiology questions, USMLE STEP 3 CARDIOLOGY, uworld step 3 | 3 Comments »
Posted on June 27, 2018 by Archer USMLE Reviews
#492. A 37-year-old woman with a history of bulimia nervosa presents with chest pain. Patient describes it as a sharp pain, localized to the middle of the chest, and occurred acutely last night after vomiting. Current medications are fluoxetine 60 mg orally daily and a daily multivitamin.
On physical exam, patient appears ill and diaphoretic. Vital signs show temperature of 37 °C (98.6 °F), blood pressure of 135/85 mm Hg, pulse of 90 /min, respiratory rate of 30 / min, and oxygen saturation of 98% on room air. Oropharynx is erythematous, dentition is poor and back molars show significant erosion. There is dullness to percussion and diminished breath sounds over the lower lobe of the left lung. Remainder of the physical exam is normal. EKG and laboratory tests are normal. Chest x-ray shows a small left pleural effusion and evidence of pneumomediastinum.
Which of the following is the definitive diagnostic step in this patient?
A. Esophagogastroduodenoscopy
B. Barium swallow study
C. Helical CT of the chest without contrast
D. Gastrografin swallow study
E. Thoracentesis
@card-hageman
Filed under: USMLE STEP III QUESTION BANK, USMLE Test Prep | Tagged: Archer cardiology, USMLE STEP 3 CARDIOLOGY | 4 Comments »
Posted on August 9, 2017 by Archer USMLE Reviews
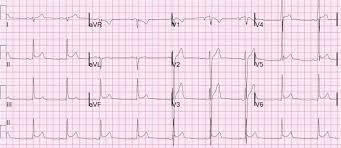
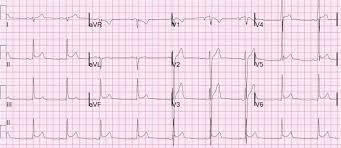
490. An 18-year-old male presents to the Emergency Department for evaluation of chest pressure for an hour. The pain is radiating to his jaw. On examination, he is diaphoretic, and he complains of nausea. Past medical history is unremarkable. Urine reveals positive benzolegonine. Below is his ECG. What is the most likely cause of the patient’s symptoms?
A. Early repolarization
B. Ischemia
C. Cocaine induced myocardial infarction
D. Atrial fibrillation
E. Wolf-Parkinson-White Syndrome
Filed under: USMLE Step 2CK Qbank, USMLE STEP III QUESTION BANK, USMLE Test Prep | Tagged: Archer cardiology, ARCHER ELECTROCARDIOGRAMS, ARCHER STEP3 LIVE REVIEWS, ARCHER STEP3 RAPID REVIEW, USMLE STEP 3 CARDIOLOGY, USMLE STEP 3 ELECTROCARDIOGRAMS, USMLE Step3, USMLE STEP3 PREPERATION | 5 Comments »
Posted on January 19, 2015 by Archer USMLE Reviews
Your patient is a 48-year-old postmenopausal female with recent onset of stage I hypertension. She has a history of osteoporosis. On exam, her blood pressure is 155/90, heart rate is 80 and regular, and respirations are 16. Cardiovascular examination is unremarkable. She has no other medical history. She has previously been controlling her hypertension with lifestyle modifications and diet. Which of the following medications is the best choice for initial pharmacological treatment of her hypertension?
A. Calcium channel blocker
B. Thiazide diuretics
C. Angiotensin receptor blocker
D. Alpha-adrenergic blocker
E. Angiotensin converting enzyme inhibitor
Filed under: USMLE STEP III QUESTION BANK, USMLE Test Prep | Tagged: Archer cardiology, archer general internal medicine, internal medicine board review, USMLE STEP 3 CARDIOLOGY | 4 Comments »
Posted on May 9, 2013 by Archer USMLE Reviews
Q437) A 65 year old man with HTN presents to your office for evaluation of right leg pain that increases on walking about one block. The pain seems to disappear when he sits and takes rest for about 10 minutes. He is concerned because it is interfering with his exercise activity that his cardiologist has recommended him. His medications include hydrochlorthiazide and enalapril. The patient has a history of heavy smoking but he quit 2 years ago. Physical exam was normal except for diminished dorsalis pedis pulses bilaterally. An arterial doppler is performed and ankle brachial index obtained which is 0.70 . The next best step in the management of his leg pain?
A) Start Cilostozol
B) Start Pentoxyfilline
C) Supervised exercise therapy
D) Recommend unsupervised exercise for 30 minutes everyday.
E) Add clopidogrel.
F) Obtain Magnetic Resonance Angiography.
G) Arterial bypass surgery
438) For the patient in Q437, which of the following is most effective in reducing the combined risk of ischemic stroke, myocardial infarction, or vascular death ?
A) Aspirin
B) Clopidogrel
C) Cilostozol
D) Pentoxifilline
E) Abciximab
439) The patient was appropriately treated and a follow up visit was scheduled one month later. The patients symptoms have moderately improved. During this visit, his fasting lipid panel revealed an LDL of 126mg%, HgbA1c of 5.5 and a blood pressure of 128/82. Next important step:
A) Advise dietary modification to treat his high LDL cholesterol
B) Start Atorvastatin and Dietary changes
C) Start Metformin
D) Start Metoprolol
440) Three months after he was diagnosed with Peripheral arterial disease, the patient suffered a massive myocardial infarction and hospitalized. He underwent Coronary artery bypass grafting and his symptoms are now well controlled. While in the hospital, the patient was started on Aspirin and Clopidogrel. He was continued on Hydrochlorthiazide and Enalapril. His Ejection fraction after the MI was 35%. One month after discharge, during a regular follow up with his cardiologist, he was started on metoprolol. Two weeks after this the patient comes back to your office with worsening leg pain on walking. On physical examination, the legs are normal in color with diminished dorsalis pedis pulses bilaterally.
Next best step in management:
A) Stop metoprolol
B) Change metoprolol to carvedilol
C) Start Cilostozol
D) Obtain angiogram and schedule arterial bypass surgery
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology | 14 Comments »
Posted on May 13, 2012 by Archer USMLE Reviews
426) A 70-year-old man with history of atrial fibrillation and metallic mitral valve presents to the out patient clinic for follow up. He has been taking warfarin for the past 5 years. His INR has been in therapeutic range between 3.0 to 4.0. However, over the last one month his INR has been in the range of 1.5 to 2.0 . His other medical problems include moderate osteoarthritis and mild cognitive dysfunction. He started taking Glucosamine supplements for “preserving his joints “and Ginseng to slow “ageing of his brain” about two months ago. He has also been started on Aspirin by his cardiologist about 1 month ago. On examination, he is afebrile and vitals are stable. Abdominal examination is benign. A repeat INR is still sub-therapeutic at 1.5. Which of the following is the most appropriate management?
A) Increase Warfarin dose by 20%
B) Stop Glucosamine and repeat INR in 1 week
C) Continue Warfarin at same dose and repeat INR in 1 week
D) Stop Ginseng and repeat INR in 1 week
E) Stop Aspirin, increase Warfarin dose and repeat INR in 1 week
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, Archer hematology, usmle hematalogy, USMLE STEP 3 CARDIOLOGY, USMLE step 3 Hematology | 21 Comments »
Posted on May 2, 2012 by Archer USMLE Reviews
418) A 76-year-old woman with history of stage III melanoma of the right lower extremity underwent a lymph node dissection about one year ago. Her other history includes Diabetes and hypertension. She presents with complaints of increasing pain in her right lower extremity for the past 2 months. The pain appears upon standing or walking down the stairs for past few weeks. Her pain gets better upon walking uphill and when she sits down to rest. There is no history of limb swelling. On examination, vitals are stable. Pulses are palpable but slightly diminished in lower extremities. Reminder of physical examination is unremarkable. Which of the following is the most appropriate diagnosis ?
A) Peripheral Artery Disease
B) Chronic Venous Insufficiency
C) Lymphedema
D) Deep Vein Thrombosis
E) Lumbar Spinal Stenosis
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, USMLE STEP 3 CARDIOLOGY | 20 Comments »
Posted on May 2, 2012 by Archer USMLE Reviews
417) A 72-year-old woman with history of stage III melanoma of the right lower extremity underwent a lymph node dissection about one year ago. Her other history includes Diabetes and hypertension. She presents with complaints of increasing pain in her right lower extremity upon walking a block for past few weeks. The pain gets better with rest. There is no history of limb swelling. On examination, vitals are stable. Physical examination is unremarkable with out any swelling or tenderness in her extremities.
Which of the following is the most appropriate diagnosis?
a) Peripheral artery disease
b) Chronic Venous insufficiency
C) Lymphedema
d) Deep Vein Thrombosis
e) Phlegmasia Alba Dolens
Which of the following is indicated next?
A) Venous Doppler
B) Compression Stockings
C) Clopidogrel
D) Check blood pressure at ankle and elbow levels
E) Leg elevation
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, USMLE STEP 3 CARDIOLOGY | 12 Comments »
Posted on May 2, 2012 by Archer USMLE Reviews
416) A 60-year-old woman with history of stage III melanoma of the right lower extremity underwent a lymph node dissection about one year ago. She presents with increasing swelling and mild pain in her right lower extremity over past several months. The pain is present all the time and does not get better with rest. The swelling has progressively increased and now, she has unsightly thickening of the skin. On examination, there is non-pitting edema of the entire right lower extremity. The skin is thickened and can not be pinched and lifted.
Which of the following is the most likely diagnosis?
A) Chronic Venous Insufficiency
B) Phlegmasia Alba Dolens
C) Phlegmasia Cerulea Dolens
D) Lymphedema
D) Peripheral Arterial Disease
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, USMLE STEP 3 CARDIOLOGY | 11 Comments »
Posted on May 2, 2012 by Archer USMLE Reviews
415) A 60-year-old woman with history of stage III melanoma of the right lower extremity underwent a lymph node dissection about one year ago. Her other history includes Diabetes and hypertension. She presents with complaints of increasing pain in her right lower extremity upon walking. The pain gets better with rest. On examination, there is mild swelling of her right extremity with a 2 cm very shallow, clean, weeping ulcer on the medial malleolus with granulation tissue in the base. There is hyperpigmentation surrounding the ulcer. There is no “pitting” of the swelling and the skin can be easily lifted from the subcutaneous tissues. Dorsalis pedis and posterior tibial artery pulses are mildly diminished.
Which of the following is indicated for her ulcer at this time?
A) Leg elevation and absorbent dressing
B) Antibiotics
C) Compression stockings
D) Anti-coagulation
E) Angiography
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, USMLE STEP 3 CARDIOLOGY | 10 Comments »
Posted on May 2, 2012 by Archer USMLE Reviews
414) A 62-year-old software engineer presents with complains of mild pain and swelling in his right lower extremity which has been progressively increasing over the past 6 months. The swelling is more towards the end of the day. Pain is worse on walking or standing and gets better with rest. On examination, vitals are stable. There is non-pitting edema of right lower extremity below the level of the knee. The limb looks normal above the level of the knee. There is some bluish discoloration of the skin over the distal portion of the leg. Small intradermal bluish vessels are noted in the skin of her right lower extremity. Dorsalis pedis and tibial pulses are intact. Which of the following is the most likely diagnosis?
A) Chronic Venous Insufficiency
B) Phlegmasia Alba Dolens
C) Phlegmasia Cerulea Dolens
D) Lymphedema
D) Peripheral Arterial Disease
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, USMLE STEP 3 CARDIOLOGY | 14 Comments »
Posted on May 2, 2012 by Archer USMLE Reviews
413) A 60-year-old woman with history of stage III melanoma of the right lower extremity underwent a lymph node dissection about one year ago. Now, she presents with pain in her right lower extremity that started about one week ago and is progressively worse. Over the last two days, she developed bluish discoloration of the right great toe . On examination, her vitals are stable. There is gross swelling of the entire right lower extremity with bluish discoloration of right great toe and extreme tenderness . Dorsalis and posterior tibial artery pulses are slightly diminished. Which of the following is the most likely diagnosis?
A) Chronic Venous Insufficiency
B) Phlegmasia Alba Dolens
C) Phlegmasia Cerulea Dolens
D) Lymphedema
D) Peripheral Arterial Disease
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, USMLE STEP 3 CARDIOLOGY | 6 Comments »
Posted on April 30, 2012 by Archer USMLE Reviews
412) An 78 year old man with history of dementia is evaluated in your office for three episodes of “syncope” over the past two months. He lives with his daughter at home. She reports that he fell to the floor and lost consciousness in the morning after getting up from his bed and the episodes would last for few minutes but he would return to his usual baseline mental status after the event. There is no history of chest pain or shortness of breath. She has seen him become increasingly “stiff” over the years and he has had worsening of tremors in his hands. When he writes, the letters are very small and difficult to decipher. He has been taking Donepezil and Memantine for Alzheimer’s for about 2 years. On examination, his pulse is 90/min, Blood Pressure 110/60 mm Hg. He has Bradykinesia and Pill rolling tremor in his hands. Cardiac examination is normal with out any murmurs. Laboratory investigations revealed a normal hemoglobin, blood glucose and electrolytes. An electrocardiogram is within normal limits. Which of the following is indicated next?
A) Orthostatic Vitals
B) 24 hour Holter-Monitoring
C) Discontinue Memantine and Donepezil
D) CT Scan of the Head
E) Tilt-Table Test
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, aRCHER GERIATRICS, USMLE STEP 3 CARDIOLOGY, usmle step 3 geriatrics | 10 Comments »
Posted on April 30, 2012 by Archer USMLE Reviews
411) An 88 year old man with history of moderate dementia is evaluated in your office for recurrent episodes of “syncope” over the past few months. There is no history of any chest pain or shortness of breath for a similar complaint. Nursing home staff reports that lately, he has been noted to be more confused than usual on several occasions and becomes very drowsy. He was sent to the Emergency Room twice last month for the same issue. There is no history of complete loss of consciousness. As per his nursing home chart, his other medical issues include poorly-controlled Osteoarthritis pain, “Sun-Downing” and Insomnia. On examination, his vitals are stable. He is currently awake. There are no focal neurological deficits. Cardiac examination is normal with out any murmurs. Laboratory investigations revealed a normal hemoglobin, blood glucose and electrolytes. An electrocardiogram is within normal limits. Which of the following is indicated next?
A) Orthostatic Vitals
B) 24 hour Holter-Monitoring
C) Electroencephalogram
D) Review of his medications
E) Tilt-Table Test
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, aRCHER GERIATRICS, USMLE STEP 3 CARDIOLOGY, usmle step 3 geriatrics | 11 Comments »
Posted on April 30, 2012 by Archer USMLE Reviews
410) A 30 year old man presents to the emergency room after having had a syncopal episode. His girl friend reports he suddenly collapsed to the floor and lost consciousness for few minutes. There was no evidence of tonic clonic movements. After regaining his consciousness, he was completely alert and awake. He reports he has had sweating and nausea prior to the episode. He has had about 2 to 3 such episodes per year for past several years. He was admitted for similar episodes in the past and telemetry monitoring was uneventful. He denied any chest pain, shortness of breath or palpitations prior to the episode. He has no other significant medical problems. On examination, his vitals are stable. He is completely awake and oriented. There are no focal neurological deficits. Cardiac examination is normal with out any murmurs. Laboratory investigations revealed a normal hemoglobin, blood glucose and electrolytes. An electrocardiogram is within normal limits. Which of the following is indicated next?
A) Holter Monitoring
B) CT scan of the Head
C) Tilt-Table testing
D) Carotid Doppler
E) Electrophysiology Study
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, USMLE STEP 3 CARDIOLOGY | 10 Comments »
Posted on April 29, 2012 by Archer USMLE Reviews
409) A 64 year old post-menopausal woman with history of hypertension and coronary artery disease presents to the Emergency Room with severe left sided chest pain that started 1 hour ago at rest. The pain radiates to her left shoulder and her jaw. Her history is significant for per-cutaneous coronary intervention to the left anterior coronary artery and placement of drug-eluting stent 9 months ago. Her medications include aspirin, Clopidogrel, Metoprolol and Lisinopril. One week ago, she had a dental extraction procedure and had discontinued Aspirin and Clopidogel prior to the procedure. She was scared of bleeding and has not resumed these medications yet. A chest X-ray is normal. An electrocardiogram reveals 5mm ST segment elevations in the anterior leads and reciprocal depressions in the inferior leads. Which of the following is the most appropriate explanation of this patient’s presentation?
A) Pericarditis
B) Re-Stenosis within the stent
C) Stent Thrombosis
D) Rupture of a new plaque in anterior coronary artery
E) Stenosis from progressive atherosclerosis of anterior coronary artery
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, USMLE STEP 3 CARDIOLOGY | 14 Comments »
Posted on April 29, 2012 by Archer USMLE Reviews
408) A 52 year old post-menopausal woman with history of hypertension, coronary artery disease and early stage breast cancer is evaluated in your office prior to breast reconstruction surgery. She was diagnosed with left breast invasive ductal carcinoma one year ago and has undergone left modified radical mastectomy followed by chemotherapy. Her history is significant for cardiac catheterization 3 months ago with coronary stent placement. Medications include Aspirin, Clopidogrel, metoprolol, lisinopril and anastrozole. She is physically active and walks about 3 blocks per day with out any chest pain or shortness of breath. Physical examination is unremarkable except fore evidence of left mastectomy. A resting electrocardiogram, chest x-ray , complete blood count and electrolytes are normal. Which of the following is the most appropriate recommendation at this time?
A) Schedule exercise stress test and if normal, clear for surgery
B) Discontinue Clopidogrel and clear for surgery
C) Obtain 2D echo and if normal, clear for surgery
D) Admit, discontinue clopidogrel, start heparin and then, proceed with surgery
E) Recommend delaying surgery at least another 8 months
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, USMLE STEP 3 CARDIOLOGY | 15 Comments »
Posted on April 23, 2012 by Archer USMLE Reviews
395) A 65 year old man with history of Hypertension, Peripheral Artery disease and Dyslipidemia is seen during a follow-up office visit. His medications include Atorvastatin 80mg, Enalapril 20mg and Clopidogrel 75 mg/ day. He does not have any new complaints and tolerating his medications well. He still smokes about 1 pack per day despite repeated counselling however, he has been strictly compliant with low-fat diet. On examination, his vitals are stable. Lower extremity dorsalis pedis are slightly diminished bilaterally. Reminder of the examination is unremarkable. A fasting lipid profile obtained a week ago showed : Total Cholesterol : 205 mg% LDL cholesterol (calculated) 90mg%, HDL – cholesterol 45 mg%, Triglycerides 350mg%. Liver function tests , Serum electrolytes, Creatinine and Complete blood count are within normal limits. Which of the following is the most appropriate next step?
A) Add Fenofibrate
B) Add Niacin
C) Add Cholestyramine
D) Change Atorvastatin to Rosuvastatin
E) Increase the dose of Atorvastatin
Filed under: Uncategorized, USMLE Test Prep | Tagged: approach to hyperlipidemia, Archer cardiology, archer preventive medicine, choosing hyperlipidemia therapy, Goals in treating hyperlipidemia, Hyperlipdemia Drugs and effects, USMLE STEP 3 CARDIOLOGY, usmle step 3 preventive medicine | 5 Comments »
Posted on April 22, 2012 by Archer USMLE Reviews
394) A 36 year old woman with Type I diabetes mellitus presents to your office because she just learned that she is pregnant. She is excited and seeks your advise. Her home blood sugars are well controlled on a basal-bolus regimen of Glargine and Lispro insulin. Her other medications include Atorvastatin and aspirin. Her most recent HgbA1C was 6.0%. Her records also reveal that her most recent fasting lipid profile met the therapeutic goals at LDL of 80mg% and Non-HDL cholesterol of 100mg%. On examination, she is comfortable. Vitals are stable and reminder of the examination is unremarkable. An office based serum pregnancy test is positive. A repeat fasting lipid profile reveals Total Cholesterol : 250 mg% LDL cholesterol (calculated) 140mg%, HDL – cholesterol 40 mg%, Triglycerides 350mg%. Liver function tests , Serum electrolytes, Creatinine and Complete blood count are within normal limitsWhich of the following is the most appropriate next step?
A) Therapeutic Abortion
B) Add Niacin to her Lipid Regimen
C) Discontinue Statin and Start Niacin
D) Discontinue Statin and advise Diet modification alone
E) Increase Atorvastatin
Filed under: Uncategorized, USMLE Test Prep | Tagged: approach to hyperlipidemia, Archer cardiology, archer ostetrics and gynecology, archer preventive medicine, choosing hyperlipidemia therapy, Goals in treating hyperlipidemia, Hyperlipdemia Drugs and effects, hyperlipidemia in pregnancy, USMLE STEP 3 CARDIOLOGY, usmle step 3 gynecology and obstetrics, usmle step 3 preventive medicine | 8 Comments »
Posted on April 21, 2012 by Archer USMLE Reviews
387) A 56 year old man with history of depression and hypertension is brought to the Emergency Room by his sister for altered mental status. There is no history of fever, nausea, vomiting or diarrhea. There is no evidence of any witnessed seizure. She is not aware of what medications he takes. On examination, he is disoriented and lethargic. He is afebrile, Pulse is 84/min, Respiratory rate 18/min, Blood pressure 80/40 mm Hg, Oxygen saturation 98%. He does not respond to verbal commands. Gag reflex is present. Respiratory examination si normal with out any wheezing, rhonchi or crepitations. Cardiac examination and abdominal exam is benign. Intravenous Naloxone and Thiamine were administered in the field without any response. An electrocardiogram is normal. Serum electrolytes and complete blood count, finger stick glucose are within normal limits. Arterial blood gases does not show any acidemia. A urine drug screen reveals:
Cocaine – Negative
Amphetamines – Negatives
Benzodiazepenes – Positive
Opiates – Negative
Cannabis – Negative
Tricyclic Anti-Depressants – positive
A suction of his airway and central line are placed and he is started on intravenous fluids. His systolic blood pressure remains in 70 to 80 mm Hg range
Which of the following is the most appropriate next step?
A) Activated Charcoal
B) Intravenous Flumazenil
C) Serum Alkalinization
D) Start Norepinephrine
E) Intravenous Lidocaine
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, archer poisoning questions, drug overdose questions, poisoning, USMLE STEP 3 CARDIOLOGY, usmle step 3 poisoning questions | 24 Comments »
Posted on April 21, 2012 by Archer USMLE Reviews
386) A 54 year old man presents to the emergency room with dizziness and intermittent palpitations for the past 12 hours. He denies any syncopal episodes or headache or seizures. He has no significant cardiac history. He was seen in the outpatient clinic one week ago for pneumonia and was started on Moxifloxacin. His other medical problems include hypertension for which he is on enalapril and Gastro-esophageal reflux disease for which he takes esomoprazole. Physical examination reveals regular heart sounds and no murmurs. Complete Blood Count and Serum electrolytes are within normal limits. An electrocardiogram is obtained and is shown below:

Which of the following is the most appropriate action at this time?
A) Intravenous Magnesium sulfate
B) Discontinue Moxifloxacin
C) Discontinue Esomoprazole
D) Transvenous Pacing
E) Intravenous Isoproterenol
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, USMLE STEP 3 CARDIOLOGY | 11 Comments »
Posted on April 21, 2012 by Archer USMLE Reviews
384) A 55 year old airline pilot presents for a follow-up visit for hypertension. He was diagnosed with hypertension a year ago and has been on treatment with hydrochlorthiazide and lisinopril. He denies any chest pain, palpitations or shortness of breath on exertion. He has no other significant health issues. His Hemoglobin a1C about 6 months ago was 5.0% . A lipid profile obtained 3 months ago showed a total chlesterol of 270mg% with HDL cholesterol of 34mg%. He smokes about 1 pack per day but denies any drug or alcohol abuse. There is no family history of Diabetes or coronary artery disease or abdominal aorta aneurysm. On examination, his blood pressure is 138/74. Cardiac examination shows regular heart sound with no S3 gallop or S4. There are no audible murmurs. Abdominal examination is benign and there are no audible bruits. A complete blood count, comprehensive metabolic panel and urinalysis are unremarkable. A resting electrocardiogram shows changes consistent with left ventricular hypertrophy. He had a colonoscopy five years ago which was normal. Which of the following is indicated at this time?
A) No additional Tests
B) Exercise Stress Test
C) Cardiac catheterization
D) Abdominal Ultrasound for Aortic aneurysm
E) Fecal Occult Blood Testing
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, archer general internal medicine, archer preventive medicine, USMLE STEP 3 CARDIOLOGY, usmle step 3 preventive medicine | 9 Comments »
Posted on April 21, 2012 by Archer USMLE Reviews
383) A 38 year old african-american male nurse is evaluated in your office because his blood pressure was found to be elevated when the doctor Employee Health Center checked his blood pressure. He was checked in the Employee Health 3 months ago and at that time, his blood pressure was 146/94 mm Hg and a repeat reading by the same doctor was 148/92 mm Hg a month ago. He checked his blood pressure at home two times at his home and it was ranging between 120/76 to 124/82. He does not trust this doctor at his work place so, he decided to come and visit you. He denies any dizziness, chest pain, palpitations or shortness of breath. He does not smoke or does not drink alcohol. Several members in family have history of Hypertension. On examination, his blood pressure is 150/94. His Body Mass Index is 26kg/m2. Cardiac examination shows regular heart sounds. There are no audible murmurs. An electrocardiogram reveals positive voltage criteria for left ventricular hypertrophy. A subsequent 2D-Echo reveals left ventricular hypertrophy with good ejection fraction at 60% and no valvular problems. Serum creatinine is 1.0mg% and Urinalysis is normal. A lipid profile has been ordered. Which of the following is the most appropriate investigation to be ordered next?
A) Exercise Stress Test
B) Ambulatory Blood Pressure Monitoring
C) Hemoglobin A1C
D) Plasma Metanephrines
E) Captopril Renal Scan
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, archer preventive medicine, USMLE STEP 3 CARDIOLOGY, usmle step 3 preventive medicine | 7 Comments »
Posted on April 21, 2012 by Archer USMLE Reviews
382) A 36 year old Caucasian man presents for a pre-employment health physical. He denies any health problems in the past. He does not smoke or drink alcohol. He denies drug abuse. He enjoys good health and has no significant medical issues. He has no family history of Hypertension, Dyslipidemia, Diabetes or coronary artery disease. On examination, his blood pressure is 118/74. Body Mass Index is 24kg/m2. Cardiac examination shows regular heart sound with no S3 gallop or S4. There are no audible murmurs. Abdominal examination is benign and there are no audible bruits. A complete blood count, comprehensive metabolic panel, urinalysis and urine drug screen are unremarkable. Which of the following is indicated at this time?
A) No additional Tests
B) Serum Total Cholesterol and HDL – cholesterol
C) Hemoglobin A1C
D) Fasting Plasma Glucose
E) Prostate Specific Antigen
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, archer general internal medicine, archer preventive medicine, The Healthy Patient!, USMLE STEP 3 CARDIOLOGY, usmle step 3 preventive medicine | 8 Comments »
Posted on April 21, 2012 by Archer USMLE Reviews
381) A 32 year old Caucasian man is evaluated in your office for hypertension. He reports that he was first noted to have high blood pressure 6-months ago at which time the reading was 146/92 . At that time, he was asked to follow-up in the office however, he disregarded the advise. Recently, during a pre-employment check-up and again at a community health fair, he was noted to have high blood pressure above 150/90 . He denies any dizziness, chest pain, palpitations or shortness of breath. He does not smoke or does not drink alcohol. His mother was diagnosed with hypertension at 60 years of age and father has had hypertension since the age of 50. He On examination, his blood pressure is 154/98. Body Mass Index is 24kg/m2. Cardiac examination shows regular heart sound with no S3 gallop or S4. There are no audible murmurs. Abdominal examination is benign and there are no audible bruits. Femoral and radial pulses are normal with out any delay. Ophthalmological examination is normal An electrocardiogram is normal with no evidence of left ventricular hypertrophy. Serum creatinine is 1.0mg% and Urinalysis is normal. Which of the following is the most appropriate next step in evaluating his Hypertension?
A) Renal Artery Magnetic Resonance Angiography
B) 24 Hour Urinary Metanephrines
C) Plasma Renin Activity- Aldosterone Ratio
D) Ambulatory Blood Pressure monitoring
E) No additional diagnostic work-up
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, USMLE STEP 3 CARDIOLOGY | 12 Comments »
Posted on April 20, 2012 by Archer USMLE Reviews
372) A 65 year old man presents to the Emergency room with complaints of severe abdominal pain that began 30 minutes ago while at rest. He reports diffuse pain that all over his abdomen, the lower back as well as in the flanks. His past medical history is significant for diabetes mellitus and peripheral vascular disease. He denies any abdominal trauma. He smokes about 1 pack cigarettes per day . On examination, he is in severe distress secondary to pain. He is afebrile, blood pressure is 80/40 mm Hg, pulse 120/min and respiratory rate 24/min. Abdomen is mildly distended with mild tenderness and a palpable pulsatile mass. Femoral and dorsalis pedis pulses are diminished. An electrocardiogram reveals sinus tachycardia. The patient is started on intravenous fluids and is placed on a cardiac monitor. Which of the following is the most appropriate next step?
A) CT scan of the abdomen
B) Exploratory laporotomy
C) Cardiac enzymes
D) Focused Abdominal Sonography in Trauma ( FAST)
E) Start Insulin Drip.
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, ARCHER GASTROENTEROLOGY, archer surgery, USMLE STEP 3 CARDIOLOGY, USMLE STEP 3 GASTROENEROLOGY, usmle step 3 surgery | 22 Comments »
Posted on April 7, 2012 by Archer USMLE Reviews
342) A 65 year old man presents with progressively increasing shortness of breath. He has a 100 pack year history of smoking. His past medical history is significant for coronary artery disease and congestive heart failure. He has been admitted several times in the past one year for Congestive heart failure exacerbations which resulted from his non-compliance with diet and medications. His medications include aspirin, metoprolol, enalapril, and spironolactone and tiotropium inhaler. On examination, he is afebrile with respiratory rate 24/min, pulse 106beats/min, blood pressure 140/90. Crepitations are heard at bilateral lung bases and breath sounds decreased bilaterally. A 2D echocardiogram reveals ejection fraction at 30% . An EKG reveals changes consistent with left ventricular hypertrophy. A Chest X-ray shows moderate pleural effusions bilaterally. Which of the following is the most appropriate next step in management of pleural effusion?
A) Intravenous Furosemide
B) Tube Thoracostomy
C) Tube thoracostomy followed by Pleurodesis
D) Needle thoracentesis
E) Implantable Cardioverter-Defibrillator (ICD) placement
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, Archer pulmonology, USMLE STEP 3 CARDIOLOGY, USMLE STEP 3 PULMONOLOGY | 10 Comments »
Posted on April 7, 2012 by Archer USMLE Reviews
341) A 78 year old man presents with progressively increasing shortness of breath. He has a 100 pack year history of smoking. His past medical history is significant for chronic obstructive pulmonary disease, coronary artery disease and congestive heart failure. He has been admitted several times in the past one year for Congestive heart failure exacerbations which resulted from his non-compliance with diet and medications. His medications include aspirin, metoprolol, enalapril, and spironolactone and tiotropium inhaler. On examination, he is afebrile with respiratory rate 24/min, pulse 106beats/min, blood pressure 140/90. Breath sounds are decreased and there is dullness to percussion on the left side of the chest. Heart sounds are regular and there is no S3 gallop. A 2D echocardiogram reveals ejection fraction at 30% and a brain natriuretic peptide 250 pg/ml (Normal less than 100pg/ml) . An EKG reveals changes consistent with left ventricular hypertrophy. A Chest X-ray is shown below:

Which of the following is the most appropriate next step in management?
A) Intravenous Furosemide
B) Tube Thoracostomy
C) Intravenos Nitroglycerin
D) Needle thoracentesis
E) Implantable Cardioverter-Defibrillator (ICD) placement
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, Archer pulmonology, USMLE STEP 3 CARDIOLOGY, USMLE STEP 3 PULMONOLOGY | 10 Comments »
Posted on April 7, 2012 by Archer USMLE Reviews
340) A 52 year old woman with history of triple-negative, metastatic breast cancer presents to the Emergency Room with increasing shortness of breath. This is her third Emergency room visit in the past 2 months. Earlier, she was admitted to the hospital twice for massive pleural effusion and underwent therapeutic thoracentesis. She was told that the cancer had spread to her lungs and pleura. She received multiple courses of chemotherapy in the past and her cancer has progressed despite initial response to chemotherapy. Her oncologist recommended palliative care. On examination, she is afebrile, respiratory rate is 24/min, Blood pressure 120/70 mm Hg and Heart Rate 106/min. Breath sounds are decreased on right side of the chest. D-dimer level is 60ng/ml ( normal < 500 ng/ml) . A chest X-ray is shown below:

Which of the following management options is most appropriate for this patient?
A) Obtain Pleural biopsy
B) Tube thoracostomy and Pleurodesis
C) Start Heparin and obtain CT Angiogram
D) Pleuro-perintoneal shunt
E) Repeat Therapeutic thoracentesis
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, Archer oncology, archer palliative care, Archer pulmonology, Archer radiology, USMLE STEP 3 CARDIOLOGY, USMLE STEP 3 ONCOLOGY, usmle step 3 palliative care, USMLE STEP 3 PULMONOLOGY, USMLE STEP 3 RADIOLOGY | 17 Comments »
Posted on April 3, 2012 by Archer USMLE Reviews
339) A 55 year old man presents to the Emergency Room with complaints of swelling of his face and worsening cough for the past two days. Swelling increases on lying down. He complaints of shortness of breath for past 2 hours. He has no significant past medical problems. He smoked about 1 pack per day for the past 25 years and consumes alcohol socially. On examination, he is in moderate respiratory distress with audible, loud Stridor. His face is grossly swollen and the veins over the neck, anterior chest and the face are engorged. On auscultation, there are no crepitations, s1 and s2 are regular and normal and there is no s3 gallop . A chest X-ray is shown below:

Which of the following is the most appropriate next step in management?
A) Radiation Therapy
B) Chemotherapy
C) CT guided Per-cutaneous Needle Biopsy
D) Video-Assisted Thoracoscopic Surgery (VATS)
E) Epinephrine
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, Archer oncology, Archer pulmonology, Archer radiology, USMLE STEP 3 CARDIOLOGY, USMLE STEP 3 ONCOLOGY, USMLE STEP 3 PULMONOLOGY, USMLE STEP 3 RADIOLOGY | 9 Comments »
Posted on April 3, 2012 by Archer USMLE Reviews
338) A 65 year old man presents to the Emergency Room with complaints of swelling of his face and worsening cough for the past two days. Swelling increases on lying down. He has no significant past medical problems. He smoked about 1 pack per day for the past 45 years and consumes alcohol socially. On examination, his vitals are satble with a blood pressure of 130/80 mm Hg. His face is grossly swollen and the veins over the neck, anterior chest and the face are engorged. There is no stridor. There is no laryngeal edema. Chest is clear to auscultation bilaterally. Cardiovascular examination shows normal s1 and s2 and there is no s3 gallop . A chest X-ray is shown below:

Which of the following is the most appropriate next step in management?
A) Radiation Therapy
B) Chemotherapy
C) CT guided Per-cutaneous Needle Biopsy
D) Video-Assisted Thoracoscopic Surgery (VATS)
E) Endotracheal Intubation
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, Archer oncology, Archer pulmonology, Archer radiology, USMLE STEP 3 CARDIOLOGY, USMLE STEP 3 ONCOLOGY, USMLE STEP 3 PULMONOLOGY, USMLE STEP 3 RADIOLOGY | 12 Comments »
Posted on April 1, 2012 by Archer USMLE Reviews
337) A 62 year old man with past medical history of hypertension is admitted with bright red bleeding per rectum. He has no pain. He had four other episodes of bright red bleeding in the past one year. All the episodes were painless. He refused colonoscopy at that time. He denies any constipation or diarrhea. He reports no weight-loss. He denies any chest pain or shortness of breath. On physical examination, his vitals are stable. Cardiovascular examination reveals a 4/6 early peaking systolic murmur that radiates to his neck and the carotids. Reminder of his exam is benign. The patient agrees for endoscopic evaluation and is scheduled for Colonoscopy. Which of the following is most likely to be diagnosed on Colonoscopy?
A) Ischemic Colitis
B) Colon cancer
C) Diverticulosis
D) Arterio-Venous Malformations
E) Internal Hemorrhoids
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, ARCHER GASTROENTEROLOGY, USMLE STEP 3 CARDIOLOGY, USMLE STEP 3 GASTROENEROLOGY | 12 Comments »
Posted on April 1, 2012 by Archer USMLE Reviews
336) A 21 year old hispanic woman is evaluated in your office for recently diagnosed Hypertension. On previous two visits, her blood pressure was 150/90 mm HG. She denies any family history of Hypertension. Her Past medical history is significant for multiple Urinary tract infections and enuresis as a child. She has no other complaints. On examination, her repeat blood pressure is 148/92 mm HG. There are no abdominal bruits. Ultrasonography reveals scarring of both kidneys. Which of the following is an important feature of this condition?
A) Positive Anti-DsDNA
B) Strong Genetic Pre-disposition
C) Association with Berry aneurysms
D) Postural Hypotension
E) Abdominal Striae
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, ARCHER NEPHROLOGY, archer pediatrics, dr.red nephrology lecture, USMLE STEP 3 CARDIOLOGY, usmle step 3 nephrology, USMLE STEP3 PEDIATRICS | 14 Comments »
Posted on March 31, 2012 by Archer USMLE Reviews
333) A 75 year old woman with past medical history of Type 2 Diabetes mellitus, Hypertension and Ischemic stroke presents to your office for a new patient visit. She has been under the care of another primary care physician who has retired from practice so the patient has decided to establish care with you. She has left sided residual weakness from her old cerebrovascular accident. She has no other complaints. She requests you for a refill of warfarin which she has been taking for three years . This drug was prescribed by her former physician for “stroke prevention” . Her recent echcardiogram shows an ejection fraction of 60% and a recent cardiovascular stress test was negative for ischemia. Her other medications include Metformin, Glyburide and enalapril. Her laboratory investigations including complete blood count are normal and her INR is 1.5. Which of the following is the most appropriate management?
A) Increase warfarin to achieve a target INR of 2.0 to 3.0
B) Discontinue Warfarin and start Aspirin/Dipyridamole combination
C) Continue low-dose Warfarin with target INR 1.5 to 2.0
D) Add Aspirin to her current regimen
E) Add Clopidogrel to her current regimen
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, archer neurology, neurology mcqs, USMLE STEP 3 CARDIOLOGY, usmle step 3 neurology | 12 Comments »
Posted on February 28, 2012 by Archer USMLE Reviews
327) A 16 year old boy presents to your office for a Pre-participation sports physical examination. He is healthy and physically active and has no complaints. He has no chest pain or shortness of breath. He denies any drug use or smoking. His maternal grandfather recently died suddenly of cardiac arrest from severe Myocardial Infarction at age 82. On physical examination, he is afebrile, pulse 82/min, Respiratory rate 18/min and blood pressure 106/76 mm Hg. Chest is clear to auscultation. Cardiac examination reveals a mid-systolic murmur, grade 2/6 heard best along the left sternal border. The murmur decreases in intensity when he stands and increases when he is supine. S1 and S2 are normal. The second heart sound is physiologically split. Cardiac impulse and carotid pulses are normal. The most appropriate action at this time:
A) Clear the patient for Sports participation
B) Refer to cardiology
C) Obtain 2D-Echocardiogram
D) Schedule Exercise Stress Test
E) Obtain Complete blood count
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, archer pediatrics, archer sports medicine, USMLE STEP 3 CARDIOLOGY, usmle step 3 sports medicine, USMLE STEP3 PEDIATRICS | 19 Comments »
Posted on February 7, 2012 by Archer USMLE Reviews
320) A 65 – year-old woman is evaluated in your office during a follow-up visit. Her medical problems include Diabetes mellitus type II and hypertension. She is being managed on oral metformin, glyburide and hydrochlorthiazide. Her most recent hemoglobin A1C is 6.5%. Her urine was negative for microalbumin three months ago. Her past medical history is significant for hospitalization for angioedema which occured after initiation of Enalapril three years ago. Physical examination is unremarkable. The patient requests if she can be started on Angiotensin Receptor Blocker ( ARB) because she read about its beneficial effects in preventing kidney damage in diabetics. Which of the following is the most appropriate response?
A) “You are correct. I will start you on ARB”
B) ” You can not be started on ARB because of history of Angioedema”
C) “You can start ARB but need pre-medication with steroids”
D) ” You can start ARB but there is a small risk of Angioedema”
E) ” Hydralazine/ Nitrate combination offers similar reno-protective effect as ARB”
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, ARCHER NEPHROLOGY, dr.red nephrology lecture, USMLE STEP 3 CARDIOLOGY, usmle step 3 nephrology | 9 Comments »
Posted on January 30, 2012 by Archer USMLE Reviews
318) A 55 year old woman underwent a debulking surgery with total abdominal hysterectomy, Salpingo-oophorectomy, omentectomy and appendicectomy for a recently diagnosed Stage IIIC Epithelial Ovarian Cancer. Her intra-operative course was complicated by severe blood loss and she received about 15 units of Packed Red Blood Cells. She is currently in the intensive care unit. Six hours after surgery, her blood pressure drops to 80/50 mm Hg. On examination, she is afebrile. She is drowsy but can be awakened. She denies any chest pain or shortness of breath. She has muscle tremors. Chest is clear to auscultation. Abdominal sutures are intact with no clinical evidence of Hematoma. An electrocardiogram is shown below:

Which of the following is the most likely explanation of the patient’s acute findings?
A) Hyperkalemia
B) Acute Myocardial Infarction
C) Circulatory Overload
D) Transfusion Associated Acute Lung injury
E) Citrate Toxicity
Filed under: Uncategorized, USMLE Test Prep | Tagged: ARCHER ACID-BASE, Archer cardiology, ARCHER FLUID AND ELECTROLYTES, Archer hematology, ARCHER NEPHROLOGY, dr.red nephrology lecture, Hematology, USMLE STEP 3 CARDIOLOGY, USMLE step 3 Hematology, usmle step 3 nephrology | 5 Comments »
Posted on January 30, 2012 by Archer USMLE Reviews
317) A 68-year-old african-american man with history of NYHA Class III congestive heart failure presents to your office for a follow up visit. His other medical problems include Hypertension, Stage II chronic kidney disease and Coronary artery disease. During his office visit three months ago , she was noted to have moderate hyperkalemia. At that time, his medications were adjusted which involved discontinuation of spironolactone and dose-reduction of ACE inhibitor. His other medications included Atenolol and Aspirin. She reports that she was admitted to hospital two weeks ago with severe hyperkalemia. He denies any complaints at this time. A serum potassium level is 4.5mEq/l , serum creatinine 1.8mg% and most recent echocardiogram revealed a left ventricular ejection fraction of 35% . His current medications include Atenolol, Hydrochlorthiazide and Aspirin. Which of the following is the most appropriate next step?
A) Re-start ACE inhibitor at a lower dose
B) Start Angiotensin Receptor Blocker (ARB)
C) Start Hydralazine and Isosorbide
D) Continue current medications
E) Start Spironolactone
Filed under: Uncategorized, USMLE Test Prep | Tagged: ARCHER ACID-BASE, Archer cardiology, ARCHER FLUID AND ELECTROLYTES, ARCHER NEPHROLOGY, dr.red nephrology lecture, USMLE STEP 3 CARDIOLOGY, usmle step 3 nephrology | 8 Comments »
Posted on January 30, 2012 by Archer USMLE Reviews
314) A 70-year-old man presented to the Emergency room with a 2-day history of increased thirst and frequency of urination. He reports generalized muscle weakness. His past medical history is significant for hypertension, diabetes mellitus and Stage III chronic kidney disease. His medications include Insulin Glargine, Lispro insulin, Enalapril , Atenolol and Spironolactone. Laboratory investigations reveal
Blood glucose 400mg%
Sodium 130 mEq/L
Potassium 7.5 mEq/L
Bicarbonate 26mEq/L
Chloride 100mEq/L
Creatinine 4.2mg%
An electrocardiogram is shown below:

Which of the following is the most appropriate next step?
A) Reduce the dose of Enalapril
B) Hemodialysis
C) Insulin Intravenous
D) Calcium Gluconate IV
E) Sodium biacrbonate IV
Filed under: Uncategorized, USMLE Test Prep | Tagged: ARCHER ACID-BASE, Archer cardiology, ARCHER ELECTROCARDIOGRAMS, ARCHER FLUID AND ELECTROLYTES, ARCHER NEPHROLOGY, dr.red nephrology lecture, USMLE ELECTROCARDIOGRAMS, USMLE STEP 3 CARDIOLOGY, usmle step 3 nephrology | 11 Comments »
Posted on November 14, 2011 by Archer USMLE Reviews
274) A 76 year old obese woman with history of uncontrolled Hypertension and Type 2 Diabetes is evaluated in your office during a follow-up visit. She has history of atrial fibrillation and has been taking warfarin for stroke prevention. However, she has difficulty keeping up with her appointments for INR monitoring and does not wish to continue warfarin. Mini mental status examination reveals mild dementia. Get up and Go test does no show any increased risk of fall. She denies any active bleeding. Rest of her physical examination is unremarkable. Her INR is 1.3 and her previous INRs have been sub-therapeutic. Laboratory investigations including complete blood count, serum creatinine and liver function tests are within normal limits. Which of the following management options is most appropriate for this patient?
A) Aspirin alone
B) Aspirin and Dipyridamole
C) Reduced intensity warfarin
D) Low Molecular Weight Heparin
E) Dabigatran
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, Archer hematology, archer preventive medicine, stroke prevention, USMLE STEP 3 CARDIOLOGY, USMLE step 3 Hematology, usmle step 3 preventive medicine | 7 Comments »
Posted on September 17, 2011 by Archer USMLE Reviews
260 ) A 30 year old woman is evaluated in your office during a routine antenatal visit. Her previous pregnancy 2 years was uneventful. She is now presenting at 12 week gestation. The patient has been compliant with antenatal vitamin supplements. She reports mild early morning nausea and vomiting. On physical examination, her vitals are with in normal limits. Cardiovascular examination reveal exaggerated heart sounds ( S1 and S2) and a new systolic ejection murmur across the lower left sternal border. An S3 gallop is present. A grade 1 diastolic murmur is heard at the left ventricular apex that increases in the left lateral decubitus position. Which of the following cardiovascular abnormalities would be best tolerated during an otherwise normal pregnancy?
A) Mitral Stenosis with pulmonary hypertension
B) Marfan syndrome with aortic valve involvement
C) Peri-partum cardiomyopathy in prior pregnancy
D) Atrial Septal Defect, Secundum type
E) Bicuspid aortic valve with mean gradient 55mmHg.
Filed under: USMLE Test Prep | Tagged: Archer cardiology, obstetrics, USMLE STEP 3 CARDIOLOGY, usmle step 3 gynecology and obstetrics, usmle step 3 obstetrics | 5 Comments »
Posted on September 17, 2011 by Archer USMLE Reviews
258 ) A 32 year old woman is evaluated in your office during a routine antenatal visit. She is a primigravida and is now presenting at 14 week gestation. The patient has been compliant with antenatal vitamin supplements. She reports mild early morning nausea and vomiting. On physical examination, her vitals are with in normal limits. Cardiovascular examination reveal exaggerated heart sounds ( S1 and S2) and a new systolic ejection murmur across the lower left sternal border. An S3 gallop is present. A grade 1 diastolic murmur is heard at the left ventricular apex that increases in the left lateral decubitus position. There is an exaggerated drop in systemic blood pressure by 16m Hg during inspiration ( Pulsus paradoxus). Which of the following physical examination findings in this patient is most likely to be pathological?
A) New Systolic murmur
B) Pulsus paradoxus
C) S3 gallop
D) Diastolic murmur
E) Exaggerated heart sounds
Filed under: USMLE Test Prep | Tagged: Archer cardiology, obstetrics, Physical examination, USMLE STEP 3 CARDIOLOGY, usmle step 3 gynecology and obstetrics, usmle step 3 obstetrics | 6 Comments »
Posted on September 17, 2011 by Archer USMLE Reviews
257) A 72 year old man with history of Diabetes Mellitus is rushed to the emergency room by the EMS 30 minutes after he collapsed at his home with severe left sided chest pain. Upon arrival, the patient was found to have very low blood pressure at 70/40 mm Hg. Chest examination revealed diffuse coarse crepitations. An electrocardiogram showed ST elevations in the anterior leads with reciprocal depressions. The patient was immediately started on Aspirin, GP IIb/IIIA inhibitors, Clopidogrel and Heparin. He is placed on 50% 02 by Venturi mask and his oxygen saturation on this supplemental oxygen is 92%. A diagnosis of cardiogenic shock and pulmonary edema is made and the patient is admitted to intensive care unit. The patient is placed on Intra-Aortic Balloon Counterpulsation Pump (IABP) and is rushed to cardiac catheterization lab. In which of the following situations, IABP confers more harm than benefit?
A) Acute Mycocardial Infarction (MI) with Cardiogenic Shock
B) Aortic dissection with aortic regurgitation
C) Severe left ventricular failure with pulmonary edema
D) Post-MI Ventricular Septal Perforation
E) Post-MI Acute Mitral Regurgitation
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, Archer Critical Care, cardiogenic shock, USMLE STEP 3 CARDIOLOGY, usmle step 3 critical care | 7 Comments »
Posted on September 7, 2011 by Archer USMLE Reviews
256) A 72 year old man with history of Diabetes Mellitus is rushed to the emergency room by the EMS 30 minutes after he collapsed at his home with severe left sided chest pain. Upon arrival, the patient was found to have very low blood pressure at 70/40 mm Hg. Chest examination revealed diffuse coarse crepitations. An electrocardiogram showed ST elevations in the anterior leads with reciprocal depressions. The patient was immediately started on Aspirin, GP IIb/IIIA inhibitors, Clopidogrel and Heparin. He is placed on 50% 02 by Venturi mask and his oxygen saturation on this supplemental oxygen is 92%. A diagnosis of cardiogenic shock and pulmonary edema is made and the patient is admitted to intensive care unit. If performed immediately, which of the following interventions would most likely reduce his risk of death?
A) Thrombolytic therapy
B) Dopamine infusion
C) Intra-Aortic Balloon Pump (IABP)
D) Percutaneous Coronary Intervention
E) Left Ventricular Assist Device (LVAD)
Note : SHOCK TRIAL
Filed under: Uncategorized, USMLE Test Prep | Tagged: Archer cardiology, Archer Critical Care, cardiogenic shock, USMLE STEP 3 CARDIOLOGY, usmle step 3 critical care | 17 Comments »
Posted on July 22, 2011 by Archer USMLE Reviews
242) A 64 year old man is evaluated in the clinic for moderately severe pain in his both legs for the past 6 months. He describes the pain that occurs upon standing and worse on walking. The pain is worse walking downhill and slightly less while walking uphill. He reports that the pain interferes with his activities and he has to sit for about 30 minutes each time to obtain relief from the pain. His history is significant for diabetes mellitus and chronic smoking about 1 pack per day for the past 45 years. On examination, he is afebrile and heart sounds are regular. Dorsalis pedis artery pulses are diminished bilaterally. Neurological examination is normal. Which of the following is the most appropriate next step in evaluating his pain?
A) Clopidogrel
B) Angiography
C) MRI lumbar spine
D) Ankle Brachial Index
E) Supervised Exercise
Filed under: USMLE Test Prep | Tagged: Archer cardiology, USMLE STEP 3 CARDIOLOGY | 9 Comments »
Posted on July 22, 2011 by Archer USMLE Reviews
241) A 44 year old man is evaluated in the clinic for moderately severe pain in his bilateral lower extremities for the past 6 months. He describes pain that occurs at rest and is increased on walking. The pain is worse in winters. His history is significant for chronic smoking about 2 packs per day for the past 25 years. He denies any history of thrombosis. On examination, he is afebrile and heart sounds are regular. Distal lower extremities are tender to touch. An ulcer measuring 2cm is noted on the left great toe. Posterior tibial and dorsalis pedis artery pulses are diminished. There is erythema and tenderness along the course of great saphenous vein. Laboratory investigations including complete blood count, chemistry panel and anti-nuclear antibodies are with in normal limits. Which of the following is most helpful in distinguishing this disorder from other vaso-occlusive diseases?
A) Raynaud phenomenon
B) Superficial Phlebitis
C) Digital ulcers
D) Young age
E) Diminished arterial pulses
Filed under: USMLE Test Prep | Tagged: Archer cardiology, USMLE STEP 3 CARDIOLOGY | 9 Comments »
Posted on July 10, 2011 by Archer USMLE Reviews
230) A 72-year-old white man with history of type 2 diabetes mellitus and hypertension is evaluated in your office during a follow up visit. He was discharged 3 days ago from the hospital after undergoing diagnostic cardiac catheterization for an abnormal exercise stress test. Femoral sheath was removed three days ago. He denies any chest pain or shortness of breath. On physical examination, he is afebrile, HR 120/min and blood pressure is 120/70 mm hg. There is a new palpable mass in the right groin and systolic bruit is heard at the catheter insertion site. Dorsalis pedis and posterior tibial pulses are intact. Which of the following is the most likely diagnosis?
A) Arterio-venos fistula
B) Local Hematoma
C) Femoral artery true aneurysm
D) Hematoma in continuity with arterial lumen
E) Femoral artery thrombosis
Filed under: USMLE Test Prep | Tagged: Archer cardiology, Archer Critical Care, archer surgery, USMLE STEP 3 CARDIOLOGY, usmle step 3 critical care, usmle step 3 surgery | 9 Comments »
Posted on July 10, 2011 by Archer USMLE Reviews
229 ) A 70-year-old white man with history of poorly controlled type 2 diabetes mellitus and hypertension is evaluated in the emergency room for severe pain in the right thigh. The patient has a coronary artery disease for which he underwent cardiac catheterization with percutaneous coronary intervention 2 days ago. He denies any chest pain or shortness of breath. On physical examination, temperature is 99.2F, HR 120/min and blood pressure is 80/40 mm Hg. There is erythema at the site of cardiac catheterization in the femoral area. Laboratory studies reveal a creatinine of 4.2mg% as opposed to his baseline creatinine of 1.8mg% one week ago. Which of the following is the most likely diagnosis?
A) Toxic shock syndrome
B) Atheroembolism
C) Contrast Nephropathy
D) Ruptured femoral artery pseudo-aneurysm
E) Retroperitoneal bleeding
Filed under: USMLE Test Prep | Tagged: Archer cardiology, Archer Critical Care, ARCHER NEPHROLOGY, dr.red nephrology lecture, USMLE STEP 3 CARDIOLOGY, usmle step 3 critical care, usmle step 3 nephrology | 14 Comments »
Posted on July 10, 2011 by Archer USMLE Reviews
228 ) A 70-year-old white man with type 2 diabetes mellitus and hypertension is evaluated in the emergency room for lacy purplish discoloration of the lower extremities that developed few hours ago. He reports diffuse bodyaches and low grade fever. He denies chest pain or shortness of breath. His past medical history is significant for coronary artery disease for which he underwent cardiac catheterization with percutaneous coronary intervention one week ago. He has a history of chronic atrial fibrillation for which he is on 5mg coumadin daily. His most recent INR has been therapeutic at 2.5. Physical examination reveals lacy purplish pattern on bilateral lower extremities shown in the image below.

The site of cardiac catheterization in the femoral area is clean and healing with out any tenderness or erythema. Neurological examination is normal. Laboratory studies reveal a creatinine of 4.2mg% as opposed to his baseline creatinine of 1.8mg% one week ago. Hemoglobin and platelet count are within normal limits. WBC count is 12.6k/µl with neutrophils 70%, bands of 2% , eosinophils 18% and lymphocytes 10%. Which of the following is the most likely diagnosis?
A) Toxic shock syndrome
B) Atheroembolism
C) Contrast Nephropathy
D) Anti-Phospholipid antibody syndrome
E) Cryoglobulinemia
Filed under: USMLE Test Prep | Tagged: Archer cardiology, Archer Critical Care, ARCHER NEPHROLOGY, dr.red nephrology lecture, USMLE STEP 3 CARDIOLOGY, usmle step 3 critical care, usmle step 3 nephrology | 8 Comments »
Posted on July 9, 2011 by Archer USMLE Reviews
225 ) A 40 year-old man presents to office for routine follow-up visit. His past medical history is significant for hypertension for which he is on Hydrochlorthiazide. He denies any chest pain, palpitatations, shortness of breath or syncope. He is a journalist by occupation. A routine EKG is obtained and is shown below:

Which of the following is the most appropriate managment of this patient?
A) Beta-blocker
B) Catheter ablation
C) Diltiazem
D) Observation
E) Electrophysiological studies
Filed under: USMLE Test Prep | Tagged: Archer cardiology, ARCHER ELECTROCARDIOGRAMS, USMLE ECGS, USMLE EKG, USMLE ELECTROCARDIOGRAMS, USMLE STEP 3 CARDIOLOGY, usmle step 3 critical care, USMLE STEP 3 ELECTROCARDIOGRAMS | 13 Comments »
Posted on July 9, 2011 by Archer USMLE Reviews
224 ) A 38 year old man presents to the emergency room with complaints of palpitations that started 5 hours ago and are persistent. He denies having similar episodes in the past. He has no fever or shortness of breath or chest pain. His past medical history is unremarkable and he is not on any medications. On examination, blood pressure is 110/60 mmHg, heart rate 130/min, RR 20/min and temperature 98.6 F. Cardiovascular examination reveals irregularly, irregular heart rate at 140beats/min. An Electrocardiogram now is shown below :

An EKG that was done during a pre-employment health check-up upon patient’s own request two months ago is shown below:

The most appropriate next step in managing this patient:
A) Defibrillation
B) Intravenous metoprolol
C) Intravenous Diltiazem
D) Intravenous Procainamide
E) Synchronized Cardioversion
Filed under: USMLE Test Prep | Tagged: Archer cardiology, ARCHER ELECTROCARDIOGRAMS, USMLE ECGS, USMLE EKG, USMLE ELECTROCARDIOGRAMS, USMLE STEP 3 CARDIOLOGY, usmle step 3 critical care, USMLE STEP 3 ELECTROCARDIOGRAMS | 7 Comments »
Posted on July 9, 2011 by Archer USMLE Reviews
223 ) A 38 year old obese African American man presented to the emergency department with headache, blurred vision and weakness. His past medical history was unremarkable. He smoked about 1 pack per day for 20 years. On examination, this patient’s blood pressure was 210/140 mmHg, heart rate 98/min, RR 20/min and temperature 98.6 F. He is alert, awake and oriented. Physical examination is unremarkable. There are neurological deficits. Laboratory investigations showed Hemoglobin 8.2 g/dl, White cell count 10k/µl, Platelets 97000/µl, Sodium 140meq/L, Potassium 4.0meq/L, Bicarbonate 24meq/L, BUN 34 and Creatinine 3.2mg% . Further investigations included a Lactic dehydrogenase which was elevated at 900U/L and a reticulocyte count of 7.0% . A periphreral smear is shown below :

The most appropriate next step in managing this patient:
A) Fresh frozen plasma
B) Intravenous Labetalol
C) Plasmapheresis
D) Intravenous Nitroprusside
E) Hemodialysis
Filed under: USMLE Test Prep | Tagged: Archer cardiology, Archer hematology, ARCHER NEPHROLOGY, USMLE STEP 3 CARDIOLOGY, usmle step 3 critical care, USMLE step 3 Hematology, usmle step 3 nephrology | 12 Comments »
Posted on July 9, 2011 by Archer USMLE Reviews
222 ) A 70-year-old white man with type 2 diabetes mellitus, hypertension, coronary artery disease, chronic kidney disease and severe chronic obstructive pulmonary disease is admitted with increasing shortness of breath. The patient lives by himself and he has not been very compliant with his medications. On examination, he is awake and oriented, blood pressure is 230/140 . Funduscopic examination reveals papilledema. Chest exam reveals bilateral crepitations. Neurological examination is normal. An electrocardiogram reveals non specific ST segment changes. A chest x-ray shows bilateral pulmonary edema. Pulse oximetry reveals a saturation of 89% on room air. The patient is started on oxygen by nasal cannula. Laboratory studies reveal a creatinine of 4.2mg% as opposed to his baseline creatinine of 2.2mg%. Which of the following is the most appropriate next step in management?
A) Non-contrast CT Scan, head
B) Intravenous Sodium nitroprusside
C) Intravenous Labetalol
D) Fenoldapam
E) Cardiac catheterization.
Filed under: USMLE Test Prep | Tagged: Archer cardiology, Archer pulmonology, USMLE STEP 3 CARDIOLOGY, usmle step 3 critical care, USMLE STEP 3 PULMONOLOGY | 5 Comments »
Posted on July 9, 2011 by Archer USMLE Reviews
221 ) A 73-year-old white man with type 2 diabetes mellitus, hypertension, coronary artery disease is admitted with increasing shortness of breath and lower-extremity edema. A brain natriuretic peptide level is 1000 pg/ml. His medications include glyburide, aspirin, atorvastatin and enalapril. He is allergic to sulfonamides. On physical examination, he has bilateral crepitations more in the right chest. Extremity examination reveals 3+ edema bilaterally. An electrocardiogram reveals changes consistent with left venricular hypertrophy but no evidence of acute ischemia. Cardiac enzymes are negative. A chest x-ray reveals bilateral pulmonary edema. Pulse oximetry reveals a saturation of 89% on room air. The patient is started on oxygen by nasal cannula. Which of the following is the most appropriate next step in management?
A) Intubation
B) Intravenous Furosemide
C) Bilevel Positive Airway pressure (BIPAP)
D) Intravenous Ethacrynic acid
E) Cardiac catheterization.
Filed under: USMLE Test Prep | Tagged: Archer cardiology, Archer pulmonology, USMLE STEP 3 CARDIOLOGY, usmle step 3 critical care, USMLE STEP 3 PULMONOLOGY | 6 Comments »
Posted on June 25, 2011 by Archer USMLE Reviews
204) A 16 year old boy presents for pre-participation examination prior to athletic training in his college campus. He denies any history of dizziness or palpitations or shortness of breath upon exertion. He denies any syncopal episodes. His father died of cardiac arrest during a marathon at the age of 32 years. Physical examination reveals a systolic murmur that increases with valsalva maneuver. Electrocardiogram reveals changes consistent with left ventricular hypertrophy. An echocardiogram reveals asymmetric septal hypertrophy and Systolic Anterior Motion (SAM) of the Anterior Mitral Leaflet. Which of the following is an indication for Implantable Cardioverter-Defibrillator in this patient?
A) Left Ventricular Thickness of 22mm
B) Increase in blood pressure upon exercise
C) His age
D) Systolic Anterior Motion of Mitral leaflet
E) Decrease in blood pressure during exercise
Filed under: USMLE Test Prep | Tagged: Archer cardiology, archer pediatrics, archer sports medicine, USMLE STEP 3 CARDIOLOGY, usmle step 3 sports medicine | 7 Comments »
Posted on June 25, 2011 by Archer USMLE Reviews
203) A 16 year old boy presents for pre-participation examination prior to athletic training in his college campus. He denies any history of dizziness or palpitations or shortness of breath upon exertion. He denies any syncopal episodes. He denies any family history of Sudden Cardiac Death. Physical examination reveals a systolic murmur that increases with valsalva maneuver. Electrocardiogram reveals changes consistent with lEft ventricular hypertrophy. An echocardiogram reveals asymmetric septal hypertrophy and Systolic Anterior Motion (SAM) of the Anterior Mitral Leaflet. The findings are discussed with patient and he intends to participate in athletics because he does not have any symptoms. Which of the following is the most appropriate next step?
A) Clear the patient for athletic training
B) Start Beta Blocker Therapy
C) Exercise Stress Test
D) Cardiac catheterization
E) Implantable Cardioverter-Defibrillator
Filed under: USMLE Test Prep | Tagged: Archer cardiology, archer pediatrics, archer sports medicine, USMLE STEP 3 CARDIOLOGY, usmle step 3 sports medicine | 6 Comments »
Posted on June 25, 2011 by Archer USMLE Reviews
202) A 36 year old male athlete is rushed to the Emergency Room after he collapsed during a soccer game. In the Emergency Room, he is found to be in cardiac arrest and cardio-pulmonary resuscitation is begun as per ACLS protocol. There is no history of trauma during the game. As per his brother, the patient does not have any history of hypertension or diabetes or known cardiac disease.There is no family history of sudden cardiac death. Which of the following is the most common cause of sudden cardiac death in athletes with a clinical profile similar to this patient?
A) Aortic dissection
B) Idiopathic
C) Coronary artery disease
D) Hypertrophic Obstructive Cardiomyopathy
E) Valvular Heart Disease
Filed under: USMLE Test Prep | Tagged: Archer cardiology, archer sports medicine, USMLE STEP 3 CARDIOLOGY, usmle step 3 sports medicine | 5 Comments »
Posted on June 25, 2011 by Archer USMLE Reviews
201) A 16 year old male athlete is rushed to the Emergency Room after he collapsed during a basket ball match. In the Emergency Room, he is found to be in cardiac arrest and cardio-pulmonary resuscitation is begun as per ACLS protocol. A electrocardiogram reveals ventricular fibrillation which is successfully defibrillated with 200 joules. The patient is currently awake but confused. His mother is present at the bed-side and denies any family history of sudden cardiac death. Which of the following is the most common cause of sudden death in young athletes?
A) Aortic dissection
B) Long QT syndrome
C) Blunt trauma to the chest
D) Hypertrophic Obstructive Cardiomyopathy
E) Mitral valve prolapse
Filed under: USMLE Test Prep | Tagged: Archer cardiology, archer pediatrics, archer sports medicine, USMLE STEP 3 CARDIOLOGY, usmle step 3 pediatrics, usmle step 3 sports medicine | 3 Comments »
Posted on June 24, 2011 by Archer USMLE Reviews
192) A 26-year-old man is evaluated for a history of recurrent headaches and palpitations for the past one month. At this time, he has no headache or palpitations. He denies any chest pain, dizziness or shortness of breath. His past history is unremarkable except for fleshy nodules over his trunk that have been present since adolescence and have been increasing in number. On physical examination, heart rate is 102/min; blood pressure is 168/100 (Lying) and 138/90 ( Standing). Skin examination reveals freckling in the inguinal region and several fleshy tumors on his back as shown in the picture:

An Electrocardiogram reveals Sinus Tachycardia. The most appropriate next step in management of this patient?
a. Biopsy of the tumors
b. Plasma Metanephrines
c. CT Scan of the abdomen
d. Intravenous fluids
e. 24-Hour holter monitoring
Filed under: USMLE Test Prep | Tagged: Archer cardiology, archer dermatology, USMLE STEP 3 CARDIOLOGY, USMLE STEP 3 DERMATOLOGY, usmle step 3 dermatology images | 5 Comments »
Posted on June 17, 2011 by Archer USMLE Reviews
190) A 45 year old man presents to your office for follow up of his dyslipidemia that was diagnosed 6 month. His lipid panel at that time was consistent with high Total cholesterol , Low HDL and high triglyceride levels. He was instructed on dietary modification. He presents for a follow up visit today and reports that he had been strictly compliant with reduced fat diet. His social history is significant for smoking 1 pack per day for the past 25 years . He reports drinking about 1 pint vodka per day for past 10 years. He read on an online magazine that drinking alcohol would boost his “Good” cholesterol. At this time, a repeat fasting lipid profile reveals:
Total Cholesterol : 250mg%
HDL cholesterol : 35mg%
Triglycerides: 500mg%
The most important step at this time to address his lipid abnormalities:
A) Niacin
B) Gemfibrozil
C) Fenofibrate
D) Alcohol cessation
E) Smoking cessation
Filed under: USMLE Test Prep | Tagged: Archer cardiology, archer preventive medicine, archer usmle step 3, USMLE STEP 3 CARDIOLOGY, usmle step 3 preventive medicine, usmle step 3 questions | 3 Comments »